Abstract:
In light of current societal and professional concerns regarding the medicalisation of childbirth and an apparent clinical culture of anxiety and fear of litigation, emerging evidence emphasises the importance of promoting normality within clinical practice, and the need for individualised, client-centred choice and control.
This article examines the use of water immersion as a facilitator of normal labour and birth. In defining the concept of normality, the article discusses the advantages of water immersion in decreasing maternal pain and use of other analgesics, critically increasing maternal control and satisfaction, and limiting medicalised intervention need.
Furthermore, supporting the physiological advantages of relaxation and maternal movement linked to the use of water in labour,water immersion promotes improved fetal position and enhanced labour progress.
Importantly however, the article further identifies current hindering factors to facilitating water immersion implementation, critically the current lack of sound methodological evidence and research rigor regarding potential adverse neonatal outcomes.
It concludes, despite obvious promotion of normality in childbirth, that further robust qualitative and quantitative research is needed to clarify the overall appropriateness of this practice. This would help practitioners to decide if this method is safe and be more informed of the risks and benefits before recommending it to women.
Introduction
The drive towards promoting normality in labour is evident in current research and policy drivers (RCM 2013; Downe 2008). However, when reading the literature around normal birth, it is apparent that no single set of criteriarepresents an accepted definition of ‘normal labour’ (National Institute of Clinical Excellence [NICE] 2007; Royal College of Midwives [RCM] 2013).
This debate around what constitutes normality in labour has dominated research and care provision for decades, but, for the purpose of this review, the Midwifery Care Working Party (MCWP) definition will be utilised as the referent.
This definition states that ‘normal labour’ is spontaneous in onset and progression, without the use of spinal, epidural or general anaesthesia, or medicalised intervention (MCWP 2007).Of particular interest in the support of normality in labour is the issue of medicalised intervention.
For instance, environmental pressures, such as how care is co-ordinated and led,can hinder the process (Russell 2011) and has inadvertently shifted the focus away from normality. Empowering women to take the lead in their own birthing experience, gain personal control and as a result manage their pain more effectively, underpins the definition of normality, whilst also overcoming and eliminating the need for medicalisation (Royal College of Obstetricians and Gynaecologists/Royal College of Midwives (RCOG/RCM 2006).
Adequate pain relief, such as epidural and pethidine (Nystedt, Edvardsson & Willman 2004; Cho, Lee & Ernst 2010), may induce a more positive birthing experience and personal control; however such methods do not promote normality. For this reason, practices such as water immersion as a non-medicalised method of personal control, may advantageously promote such concepts.
This review aims to present an overview of current literature around the benefits and disadvantages of using such a method to manage labour pain with an emphasis on critiquing methodological strengths and weakness.
Water immersion and pain relief
Much of the research into pain relief facilitation in childbirth concentrates on comparing the outcomes of water immersion with no intervention during the first stage of labour, in the form of unblinded randomised controlled trials (RCT) (Benfield et al. 2001; Cluett, Pickering, Getliffe & Saunders 2004; Eckert, Turnbull & MacLennan 2001; Ohlsson et al. 2001).
Despite the limitation of unblinded methodology in these studies, due to the nature of the intervention, collectively they conclude that water immersion has beneficial pain relief implications in comparison with no intervention, and a positive impact on maternal control and normality.
Barbosa da Silva, Vasconcellos de Oliveira and Nobre (2009), in comparing pain relief magnitude in first stage bathing and non-bathing women, conclude that pain is less apparent, and pain progresses lower in bathing cohorts, but overall pain relief satisfaction is highly significant (Pagano et al. 2010; RCOG/RCM 2006).
However, as this study only involved nulliparous women (first time pregnant)these findings only offer limited insights intothe women’s evaluation of labour pain. The study acknowledges the implications of using such a restricted sample group in representing the entire birthing population.
Regardless of these limitations, the reported reduction in intensity of pain and use of additional analgesia, as concluded within the study’s findings, is indicative of the potential for water immersion to contribute to the promotion of normality in labour by reducing medicalisation.
This has been replicated by other studies where a decrease in opioid use (Mollamahmutoglu et al. 2012; Cluett, Nikodem, McCandlish & Burns 2009) and incidence of epidural and spinal anaesthetics (Cluett & Burns 2009; Burns et al. 2012) has been concluded.
Women’s perception of water immersion efficacymay differ prior to commencement of this activity, therefore, this could influence their perception of pain relief (Cluett, Nikodem, McCandlish & Burns 2009); further research is needed to explore this hypothesis.
One qualitative study by Maude and Foureur (2007), which involved interviews with five women who experienced water birth at different post-natal periods, suggests that the anticipation of getting into water and consequential relaxation accelerates the rate of cervical dilation.
Due to induced cardiovascular changes, any elevation in anxiety hormones is decreased by a reduction in blood pressure, further facilitated by an increased level of endorphins (Benfield 2002; Cluett et al. 2009). Relaxation and a sense of personal control as a response to this, is arguably the main basis for pain relief in water immersion.
Literature evidence agrees that pain is not eliminated by water; however, relaxation provides a release from the pain experience, and a sense of comfort and satisfaction (McNeil & Jomeen 2010). A larger range of maternal movement improves normal labour progression and there are reported improvements in fetal position and flexion (Cluett et al. 2009; Burns 2004).
However, the methodology of Maude and Foureur’s (2007) study, in conducting differently timed postpartum interviews, raises questions of recall bias, and potential changing of emotions and opinions over time.
A reduction in medicalised intervention
One point, highly illustrated within the literature, includes the impact of water immersion on the reduced need for medicalised intervention such as episiotomy and induction (Burns et al. 2012; Geissbuehler, Stein & Eberhard 2004). Mollamahmutoglu et al. (2012) report that water immersion results in a shorter second stage of labour,with the need for induction of labour being significantly decreased.
In connection to facilitating normality through a more natural birthing process, large observational retrospective studies, such as Burns et al. (2012), conclude thata reduced need for medicalised interventions is also more prevalent in midwifery-led home water births. Care within the home is arguably another factor in facilitating normality for the birthing woman. However, a lack of a control group for this particular study, limits the reliability of this study’s conclusions.
Second and third stage management and physiological advantages
Despite water being recommended by national guidance (NICE 2007), there appears to be a small amount of evidence available that concerns labouring in water in the first and second stages. Further water immersion research is needed around these stages of labour, especially in relation to risks associated with delivery of the third stage of labour in water.
However, research undertaken with women who have had a water birth, shows a reduction in maternal adverse outcomes and need for specialised care, compared with vaginal delivery controls. A reduced incidence of perineum tears (Burns et al. 2012), maternal infections (Benfield et al. 2001) and postpartum haemorrhage (Mollamahmutoglu et al. 2012; Benfield 2002), are some of the reported outcomes,all of which promote normality and could, in addition, improve the pain experience.
Definition discrepancies
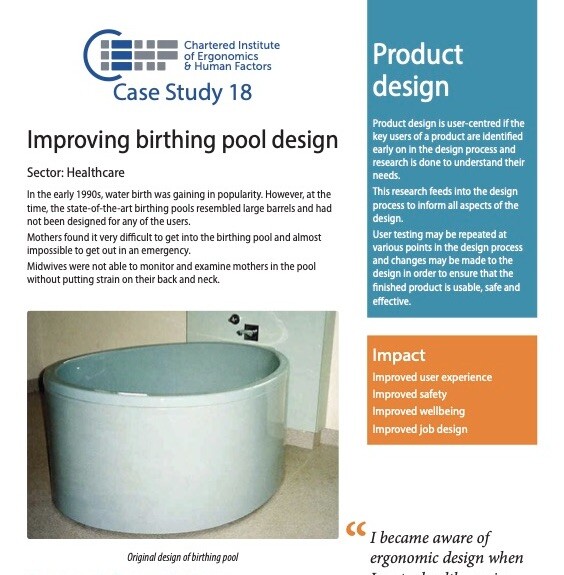
In analysis of the evidence, various definitions for water immersion can be identified, indicating a lack of homogeneity in research literature. Differences in the size of baths/pools, the depth of water and length of time exposed to the intervention, all contribute significantly to the degree of exposure experienced; however, little attention to date has been paid to these factors. Benfield et al. (2001) conducted a RCT study which exposed its participants to water for exactly an hour.
This, therefore, increased the consistency of their exposure findings; however,the authors state that the pool was shallow in comparison to those generally used on labour wards, thereby limiting the reliability and appropriateness of their findings to practice. Other studies also highlight similar weaknesses. Eckert et al. (2001) used a larger pool during its intervention; however, exposure time varied according to the woman’s preference.
Significantly, this study also allowed its control group the option of a shower, thereby introducing bias and limiting the reliability of the findings, as exposure to a shower may also have similar pain relief properties as water immersion (Stark & Miller 2009).
Barriers to practice implementation
Interestingly, one factor apparent within the evidence is the lack of investigation into the effects of temperature control, including inconsistencies in temperatures usage and the effect on any potential outcomes. NICE (2007) recommends a water temperature no higher than 37.5c, and advises this should be monitored hourly to ensure maternal comfort and apyrexia (absence of a fever).
Eckert et al. (2001) recognised the importance of temperature control in their RCT study; however,they concludedthat only 50 per cent of the 85 women in the intervention group had their temperatures recorded hourly. In comparison, Benfield et al (2001) assessed water temperature on strict fifteen minute intervals; however, the temperature was allowed to escalate as high as 38c.
Taking these inconsistencies into account, analysis of the overall literature regarding temperature control and potential pain relief is difficult, and the ability to comment on this specific factor and its relevance in facilitating normal labour remains limited. Evidently, further research is needed in order to eliminate the discrepancies in the methodology, thereby allowing results to be more comparable.
Directly linked to the issue of temperature monitoring is the importance of fetal monitoring. Interestingly, only one study has been found that specifies how fetal heart monitoring was conducted during labour (Mollamatutoglu et al. 2012). On the other hand, a quantitative study conducted by Carpenter and Weston (2012), investigating the differences between respiratory distress in water and land birth neonates, concludes that, despite no significant difference in initial APGAR scores, water immersed neonates have more severe abnormal changes identified through x-ray.
As this study involved a higher proportion of water birth inspected x-rays in comparison to land birth, this limits the rigor of the methodology, and the exclusion of co-morbidities, such as encephalopathy and congenital heart disease, indicates potential confounding factors. However, the study does conclusively identify the need of further research into potential adverse neonate outcomes after initial APGAR assessment.
The lack ofstudies into this phenomenon is widely recognised in the literature; the only study to extend assessment over the immediate neonatal period was conducted by Cluett et al. (2004), and thisstudied babies only up to day ten postpartum. Higher incidence of resuscitation (Eckert et al. 2001) and near-drowning (Pinette, Wax & Wilson 2004) further question water immersion as a safe facilitator of normal birth; however, conclusive evidence regarding neonate outcomes is scarce to date; a reliable evidence-based recommendation for practice can only be made once further research has been conducted.
Potentially the largest barrier to water immersion provision so far, does not involve the actual use of water, but the attitudes of the professionals in general and midwives in particular towards its use. Lack of confidence, limited training and pressures from the ward environment seem, on occasions, to override the professional requirement for midwives to facilitate a woman’s choice (Russell 2011).
Working in a medical environment, which super-values intervention over the promotion of a natural birth, has also been identified as an important barrier (Russell 2011).Subsequently, it can be inferred that institutional factors are key in influencingtheuse of water immersion and its potential role in normality facilitation.
However, the study by Russell (2011) only used a small sample size and findings cannot be readily generalised across the NHS or the entire midwifery profession. Other studies scoping current practice would help understand the use of water in labour in the UK.
Conclusion
As concluded by the current evidence base, research literature largely concurs that water immersion during the first stage of labour is a beneficial, natural method of pain relief.
This is due to a decreased need for medicalised interventions and additional analgesia, and an increase in personal control and relaxation, consequently facilitating normality in childbirth.
Lack of evidence on the latter stages of labour, the influence that temperature might have on the labour and/or the baby, and the implications of bathing tub dimensions, require that well conducted, methodologically strong and varied studies of all potential outcomes are carried out.
Despite numerous gaps in the evidence, one significant, largely inconclusive area remains: the lack of research into adverse neonatal outcomes and, specifically, any longer term detrimental effects. Achieving a better understanding of those, could prove advantageous in increasing the uptake of water immersion during labour as facilitator of normality in childbirth.
References
Barbosa da Silva, F.M., Vasconcellos de Oliveira, S.M.J. & Nobre, M.R.C. 2009. ‘A randomised controlled trial evaluating the effect of immersion bath on labour pain’, Midwifery 25, 286-294.
Benfield, R.D. 2002. ‘Hydrotherapy in labor’, Journal of Nursing Scholarship 34(4), 347-352.
Benfield, R.D., Herman, J., Katz, V.L., Wilson, S.P.& Davis, J.M. 2001. ‘Hydrotherapy in Labor’, Research in Nursing & Health 24, 57-67.
Burns, E.E., 2004. ‘Water: what are we afraid of?’, The Practising Midwife 7(10), 17-19.
Burns, E.E., Boulton, M.G., Cluett, E., Cornelius, V.R. & Smith, L.A. 2012. ‘Characteristics, interventions, and outcomes of women who used a birthing pool: a prospective observational study’, Birth 39(3), 192-202.
Carpenter, L. & Weston, P. 2011. ‘Neonatal consequences from water birth’, Journal of Paediatrics and Child Health 48, 419-423.
Cho, S.H., Lee, H. & Ernst, E. 2010. ‘Acupuncture for pain relief in labour: a systematic review and meta-analysis’, An International Journal of Obstetrics and Gynaecology 117, 907-920.
Cluett, E.R. & Burns, E.E. 2009. ‘Immersion in water in labour and birth’, Cochrane Database of Systematic Reviews 2, 1-56.
Cluett, E.R., Pickering, R.M., Getliffe, K, & Saunders, N.J.S.G. 2004. ‘Randomised controlled trial of labouring in water compared with standard of augmentation for management of dystocia in first stage of labour’, British Medical Journal 328(7435), 1-6.
Cluett, E.R., Nikodem, C.V.C., McCandlish, R.E. & Burns, E.E. 2009. ‘Immersion in water in pregnancy, labour and birth’, Cochrane Database of Systematic Reviews 1, 1-33.
Downe, S. 2008. Normal Childbirth, evidence and debate (2nd edition). Oxford: Churchill Livingstone.
Eckert, K., Turnbull, D. & MacLennan, A. 2001. ‘Immersion in water in the first stage of labour: a randomised controlled trial’, Birth 28(2), 84-93.
Geissbuehler, V., Stein, S. & Eberhard, J. 2004. ‘Waterbirths compared with landbirths: an observational study of nine years’ Journal of perinatal medicine 32(4), 308-314.
Maternity Care Working Party. 2007. ‘Making normal birth a reality-consensus statement from the Maternity Care Working Party-our shared views about the need to recognise, facilitate and audit normal birth’. London: Maternity Care Working Party.
Maude, R.M. & Foureur, M.J. 2006. ‘It’s beyond water: stories of women’s experiences of using water for labour and birth’, Women and Birth 20, 17-24.
McNeil, A. & Jomeen, J. 2010. ‘“Gezellig”: a concept for managing pain during labour and Childbirth’, British Journal of Midwifery 18(8), 515-520.
Mollamahmutoglu, L., Moraloglu, O., Ozyer, S., Su, F.A., Karayalcin, R., Hancerlioglu, N.,Uzunlar, O., & Dilmen, U. 2012. ‘The effects of immersion in water on labor, birth and newborn and comparison with epidural analgesia and conventional vaginal delivery’, Journal of Turkish German Gynecological Association 13, 45-49.
National Institute of Clinical Excellence (NICE). 2007. ‘Intrapartum care-care of healthy women and their babies during childbirth’. London: National Institute of Clinical Excellence.
Nystedt, A., Edvardsson, D., & Willman, A. 2004. ‘Epidural analgesia for pain relief in labour and childbirth- a review with a systematic approach’, Journal of Clinical Nursing 13, 455-466.
Ohlsson, G., Buchhave, P., Leandersson, U., Nordstrom, L., Rydhstrom, H. & Sjolin, I. 2001. ‘Warm tub bathing during labor: maternal and neonatal effects’, Acta Obstetricia et Gynecologica Scandinavica 80(4), 311-314.
Pagano, E., De Rota, B., Ferrando, A., Petrinco, M., Merletti, F., Gregori, D. 2010. ‘An economic evaluation of water birth: the cost-effectiveness of mother well-being’, Journal of Evaluation in Clinical Practice 16, 916-919.
Pinette, M.G., Wax, J. & Wilson, E. 2004. ‘The risks of underwater birth’, American Journal of Obstetrics and Gynecology 190, 1211-1215.
Royal College of Midwives (RCM). 2013. ‘Campaign for Normal Birth’. Available online at: http://www.rcmnormalbirth.org.uk/about-the-campaign/definitions-and-the-rcm-position-paper
Royal College of Obstetricians and Gynaecologists/Royal College of Midwives (RCOG/RCM). 2006. ‘Immersion in water during labour and birth’. London: Royal College of
Obstetricians and Gynaecologists and Royal College of Midwives.
Russell, K. 2011. ‘Struggling to get into the pool room? a critical discourse analysis of labor ward midwives’ experiences of water birth’, International Journal of Childbirth 1(1), 52-60.
Stark, M.A. & Miller, M.G. 2009. ‘Barriers to the use of hydrotherapy in labor’, Journal of Obstetric, Gynecologic, & Neonatal Nursing 38, 667-675.