Water Systems – Health Technical Memorandum: Department of Health
Guidance on design, installation, commissioning, testing, monitoring and operation of water supply systems in healthcare premises.
This Health Technical Memorandum (HTM 04-01) has now been revised into 3 parts, A, B and C.
It gives advice and guidance on the legal requirements, design applications, maintenance and operation of hot and cold water supply, storage and distribution systems in all types of healthcare premises to:
It also provides advice and guidance on the control and management of the risk posed by Legionella, Pseudomonas aeruginosa and other water borne pathogens within a healthcare setting.
Part A: covers the design, installation and commissioning
Part B: covers operational management
Part C: focuses on specific additional measures that should be taken to control and minimise the risk of Pseudomonas aeruginosa in augmented care units
It should be read in conjunction with the HSE’s Approved Code of Practice (L8) and HSG274 Part 2.
It is equally applicable to both new and existing sites.
Part A: design, installation and commissioning
Part B: operational management
Part C: Pseudomonas aeruginosa – advice for augmented care units
Supplement: performance specification D 08 – thermostatic mixing valves
Abstract:
In light of current societal and professional concerns regarding the medicalisation of childbirth and an apparent clinical culture of anxiety and fear of litigation, emerging evidence emphasises the importance of promoting normality within clinical practice, and the need for individualised, client-centred choice and control.
This article examines the use of water immersion as a facilitator of normal labour and birth. In defining the concept of normality, the article discusses the advantages of water immersion in decreasing maternal pain and use of other analgesics, critically increasing maternal control and satisfaction, and limiting medicalised intervention need.
Furthermore, supporting the physiological advantages of relaxation and maternal movement linked to the use of water in labour,water immersion promotes improved fetal position and enhanced labour progress.
Importantly however, the article further identifies current hindering factors to facilitating water immersion implementation, critically the current lack of sound methodological evidence and research rigor regarding potential adverse neonatal outcomes.
It concludes, despite obvious promotion of normality in childbirth, that further robust qualitative and quantitative research is needed to clarify the overall appropriateness of this practice. This would help practitioners to decide if this method is safe and be more informed of the risks and benefits before recommending it to women.
Introduction
The drive towards promoting normality in labour is evident in current research and policy drivers (RCM 2013; Downe 2008). However, when reading the literature around normal birth, it is apparent that no single set of criteriarepresents an accepted definition of ‘normal labour’ (National Institute of Clinical Excellence [NICE] 2007; Royal College of Midwives [RCM] 2013).
This debate around what constitutes normality in labour has dominated research and care provision for decades, but, for the purpose of this review, the Midwifery Care Working Party (MCWP) definition will be utilised as the referent.
This definition states that ‘normal labour’ is spontaneous in onset and progression, without the use of spinal, epidural or general anaesthesia, or medicalised intervention (MCWP 2007).Of particular interest in the support of normality in labour is the issue of medicalised intervention.
For instance, environmental pressures, such as how care is co-ordinated and led,can hinder the process (Russell 2011) and has inadvertently shifted the focus away from normality. Empowering women to take the lead in their own birthing experience, gain personal control and as a result manage their pain more effectively, underpins the definition of normality, whilst also overcoming and eliminating the need for medicalisation (Royal College of Obstetricians and Gynaecologists/Royal College of Midwives (RCOG/RCM 2006).
Adequate pain relief, such as epidural and pethidine (Nystedt, Edvardsson & Willman 2004; Cho, Lee & Ernst 2010), may induce a more positive birthing experience and personal control; however such methods do not promote normality. For this reason, practices such as water immersion as a non-medicalised method of personal control, may advantageously promote such concepts.
This review aims to present an overview of current literature around the benefits and disadvantages of using such a method to manage labour pain with an emphasis on critiquing methodological strengths and weakness.
Water immersion and pain relief
Much of the research into pain relief facilitation in childbirth concentrates on comparing the outcomes of water immersion with no intervention during the first stage of labour, in the form of unblinded randomised controlled trials (RCT) (Benfield et al. 2001; Cluett, Pickering, Getliffe & Saunders 2004; Eckert, Turnbull & MacLennan 2001; Ohlsson et al. 2001).
Despite the limitation of unblinded methodology in these studies, due to the nature of the intervention, collectively they conclude that water immersion has beneficial pain relief implications in comparison with no intervention, and a positive impact on maternal control and normality.
Barbosa da Silva, Vasconcellos de Oliveira and Nobre (2009), in comparing pain relief magnitude in first stage bathing and non-bathing women, conclude that pain is less apparent, and pain progresses lower in bathing cohorts, but overall pain relief satisfaction is highly significant (Pagano et al. 2010; RCOG/RCM 2006).
However, as this study only involved nulliparous women (first time pregnant)these findings only offer limited insights intothe women’s evaluation of labour pain. The study acknowledges the implications of using such a restricted sample group in representing the entire birthing population.
Regardless of these limitations, the reported reduction in intensity of pain and use of additional analgesia, as concluded within the study’s findings, is indicative of the potential for water immersion to contribute to the promotion of normality in labour by reducing medicalisation.
This has been replicated by other studies where a decrease in opioid use (Mollamahmutoglu et al. 2012; Cluett, Nikodem, McCandlish & Burns 2009) and incidence of epidural and spinal anaesthetics (Cluett & Burns 2009; Burns et al. 2012) has been concluded.
Women’s perception of water immersion efficacymay differ prior to commencement of this activity, therefore, this could influence their perception of pain relief (Cluett, Nikodem, McCandlish & Burns 2009); further research is needed to explore this hypothesis.
One qualitative study by Maude and Foureur (2007), which involved interviews with five women who experienced water birth at different post-natal periods, suggests that the anticipation of getting into water and consequential relaxation accelerates the rate of cervical dilation.
Due to induced cardiovascular changes, any elevation in anxiety hormones is decreased by a reduction in blood pressure, further facilitated by an increased level of endorphins (Benfield 2002; Cluett et al. 2009). Relaxation and a sense of personal control as a response to this, is arguably the main basis for pain relief in water immersion.
Literature evidence agrees that pain is not eliminated by water; however, relaxation provides a release from the pain experience, and a sense of comfort and satisfaction (McNeil & Jomeen 2010). A larger range of maternal movement improves normal labour progression and there are reported improvements in fetal position and flexion (Cluett et al. 2009; Burns 2004).
However, the methodology of Maude and Foureur’s (2007) study, in conducting differently timed postpartum interviews, raises questions of recall bias, and potential changing of emotions and opinions over time.
A reduction in medicalised intervention
One point, highly illustrated within the literature, includes the impact of water immersion on the reduced need for medicalised intervention such as episiotomy and induction (Burns et al. 2012; Geissbuehler, Stein & Eberhard 2004). Mollamahmutoglu et al. (2012) report that water immersion results in a shorter second stage of labour,with the need for induction of labour being significantly decreased.
In connection to facilitating normality through a more natural birthing process, large observational retrospective studies, such as Burns et al. (2012), conclude thata reduced need for medicalised interventions is also more prevalent in midwifery-led home water births. Care within the home is arguably another factor in facilitating normality for the birthing woman. However, a lack of a control group for this particular study, limits the reliability of this study’s conclusions.
Second and third stage management and physiological advantages
Despite water being recommended by national guidance (NICE 2007), there appears to be a small amount of evidence available that concerns labouring in water in the first and second stages. Further water immersion research is needed around these stages of labour, especially in relation to risks associated with delivery of the third stage of labour in water.
However, research undertaken with women who have had a water birth, shows a reduction in maternal adverse outcomes and need for specialised care, compared with vaginal delivery controls. A reduced incidence of perineum tears (Burns et al. 2012), maternal infections (Benfield et al. 2001) and postpartum haemorrhage (Mollamahmutoglu et al. 2012; Benfield 2002), are some of the reported outcomes,all of which promote normality and could, in addition, improve the pain experience.
Definition discrepancies
In analysis of the evidence, various definitions for water immersion can be identified, indicating a lack of homogeneity in research literature. Differences in the size of baths/pools, the depth of water and length of time exposed to the intervention, all contribute significantly to the degree of exposure experienced; however, little attention to date has been paid to these factors. Benfield et al. (2001) conducted a RCT study which exposed its participants to water for exactly an hour.
This, therefore, increased the consistency of their exposure findings; however,the authors state that the pool was shallow in comparison to those generally used on labour wards, thereby limiting the reliability and appropriateness of their findings to practice. Other studies also highlight similar weaknesses. Eckert et al. (2001) used a larger pool during its intervention; however, exposure time varied according to the woman’s preference.
Significantly, this study also allowed its control group the option of a shower, thereby introducing bias and limiting the reliability of the findings, as exposure to a shower may also have similar pain relief properties as water immersion (Stark & Miller 2009).
Barriers to practice implementation
Interestingly, one factor apparent within the evidence is the lack of investigation into the effects of temperature control, including inconsistencies in temperatures usage and the effect on any potential outcomes. NICE (2007) recommends a water temperature no higher than 37.5c, and advises this should be monitored hourly to ensure maternal comfort and apyrexia (absence of a fever).
Eckert et al. (2001) recognised the importance of temperature control in their RCT study; however,they concludedthat only 50 per cent of the 85 women in the intervention group had their temperatures recorded hourly. In comparison, Benfield et al (2001) assessed water temperature on strict fifteen minute intervals; however, the temperature was allowed to escalate as high as 38c.
Taking these inconsistencies into account, analysis of the overall literature regarding temperature control and potential pain relief is difficult, and the ability to comment on this specific factor and its relevance in facilitating normal labour remains limited. Evidently, further research is needed in order to eliminate the discrepancies in the methodology, thereby allowing results to be more comparable.
Directly linked to the issue of temperature monitoring is the importance of fetal monitoring. Interestingly, only one study has been found that specifies how fetal heart monitoring was conducted during labour (Mollamatutoglu et al. 2012). On the other hand, a quantitative study conducted by Carpenter and Weston (2012), investigating the differences between respiratory distress in water and land birth neonates, concludes that, despite no significant difference in initial APGAR scores, water immersed neonates have more severe abnormal changes identified through x-ray.
As this study involved a higher proportion of water birth inspected x-rays in comparison to land birth, this limits the rigor of the methodology, and the exclusion of co-morbidities, such as encephalopathy and congenital heart disease, indicates potential confounding factors. However, the study does conclusively identify the need of further research into potential adverse neonate outcomes after initial APGAR assessment.
The lack ofstudies into this phenomenon is widely recognised in the literature; the only study to extend assessment over the immediate neonatal period was conducted by Cluett et al. (2004), and thisstudied babies only up to day ten postpartum. Higher incidence of resuscitation (Eckert et al. 2001) and near-drowning (Pinette, Wax & Wilson 2004) further question water immersion as a safe facilitator of normal birth; however, conclusive evidence regarding neonate outcomes is scarce to date; a reliable evidence-based recommendation for practice can only be made once further research has been conducted.
Potentially the largest barrier to water immersion provision so far, does not involve the actual use of water, but the attitudes of the professionals in general and midwives in particular towards its use. Lack of confidence, limited training and pressures from the ward environment seem, on occasions, to override the professional requirement for midwives to facilitate a woman’s choice (Russell 2011).
Working in a medical environment, which super-values intervention over the promotion of a natural birth, has also been identified as an important barrier (Russell 2011).Subsequently, it can be inferred that institutional factors are key in influencingtheuse of water immersion and its potential role in normality facilitation.
However, the study by Russell (2011) only used a small sample size and findings cannot be readily generalised across the NHS or the entire midwifery profession. Other studies scoping current practice would help understand the use of water in labour in the UK.
Conclusion
As concluded by the current evidence base, research literature largely concurs that water immersion during the first stage of labour is a beneficial, natural method of pain relief.
This is due to a decreased need for medicalised interventions and additional analgesia, and an increase in personal control and relaxation, consequently facilitating normality in childbirth.
Lack of evidence on the latter stages of labour, the influence that temperature might have on the labour and/or the baby, and the implications of bathing tub dimensions, require that well conducted, methodologically strong and varied studies of all potential outcomes are carried out.
Despite numerous gaps in the evidence, one significant, largely inconclusive area remains: the lack of research into adverse neonatal outcomes and, specifically, any longer term detrimental effects. Achieving a better understanding of those, could prove advantageous in increasing the uptake of water immersion during labour as facilitator of normality in childbirth.
References
Barbosa da Silva, F.M., Vasconcellos de Oliveira, S.M.J. & Nobre, M.R.C. 2009. ‘A randomised controlled trial evaluating the effect of immersion bath on labour pain’, Midwifery 25, 286-294.
Benfield, R.D. 2002. ‘Hydrotherapy in labor’, Journal of Nursing Scholarship 34(4), 347-352.
Benfield, R.D., Herman, J., Katz, V.L., Wilson, S.P.& Davis, J.M. 2001. ‘Hydrotherapy in Labor’, Research in Nursing & Health 24, 57-67.
Burns, E.E., 2004. ‘Water: what are we afraid of?’, The Practising Midwife 7(10), 17-19.
Burns, E.E., Boulton, M.G., Cluett, E., Cornelius, V.R. & Smith, L.A. 2012. ‘Characteristics, interventions, and outcomes of women who used a birthing pool: a prospective observational study’, Birth 39(3), 192-202.
Carpenter, L. & Weston, P. 2011. ‘Neonatal consequences from water birth’, Journal of Paediatrics and Child Health 48, 419-423.
Cho, S.H., Lee, H. & Ernst, E. 2010. ‘Acupuncture for pain relief in labour: a systematic review and meta-analysis’, An International Journal of Obstetrics and Gynaecology 117, 907-920.
Cluett, E.R. & Burns, E.E. 2009. ‘Immersion in water in labour and birth’, Cochrane Database of Systematic Reviews 2, 1-56.
Cluett, E.R., Pickering, R.M., Getliffe, K, & Saunders, N.J.S.G. 2004. ‘Randomised controlled trial of labouring in water compared with standard of augmentation for management of dystocia in first stage of labour’, British Medical Journal 328(7435), 1-6.
Cluett, E.R., Nikodem, C.V.C., McCandlish, R.E. & Burns, E.E. 2009. ‘Immersion in water in pregnancy, labour and birth’, Cochrane Database of Systematic Reviews 1, 1-33.
Downe, S. 2008. Normal Childbirth, evidence and debate (2nd edition). Oxford: Churchill Livingstone.
Eckert, K., Turnbull, D. & MacLennan, A. 2001. ‘Immersion in water in the first stage of labour: a randomised controlled trial’, Birth 28(2), 84-93.
Geissbuehler, V., Stein, S. & Eberhard, J. 2004. ‘Waterbirths compared with landbirths: an observational study of nine years’ Journal of perinatal medicine 32(4), 308-314.
Maternity Care Working Party. 2007. ‘Making normal birth a reality-consensus statement from the Maternity Care Working Party-our shared views about the need to recognise, facilitate and audit normal birth’. London: Maternity Care Working Party.
Maude, R.M. & Foureur, M.J. 2006. ‘It’s beyond water: stories of women’s experiences of using water for labour and birth’, Women and Birth 20, 17-24.
McNeil, A. & Jomeen, J. 2010. ‘“Gezellig”: a concept for managing pain during labour and Childbirth’, British Journal of Midwifery 18(8), 515-520.
Mollamahmutoglu, L., Moraloglu, O., Ozyer, S., Su, F.A., Karayalcin, R., Hancerlioglu, N.,Uzunlar, O., & Dilmen, U. 2012. ‘The effects of immersion in water on labor, birth and newborn and comparison with epidural analgesia and conventional vaginal delivery’, Journal of Turkish German Gynecological Association 13, 45-49.
National Institute of Clinical Excellence (NICE). 2007. ‘Intrapartum care-care of healthy women and their babies during childbirth’. London: National Institute of Clinical Excellence.
Nystedt, A., Edvardsson, D., & Willman, A. 2004. ‘Epidural analgesia for pain relief in labour and childbirth- a review with a systematic approach’, Journal of Clinical Nursing 13, 455-466.
Ohlsson, G., Buchhave, P., Leandersson, U., Nordstrom, L., Rydhstrom, H. & Sjolin, I. 2001. ‘Warm tub bathing during labor: maternal and neonatal effects’, Acta Obstetricia et Gynecologica Scandinavica 80(4), 311-314.
Pagano, E., De Rota, B., Ferrando, A., Petrinco, M., Merletti, F., Gregori, D. 2010. ‘An economic evaluation of water birth: the cost-effectiveness of mother well-being’, Journal of Evaluation in Clinical Practice 16, 916-919.
Pinette, M.G., Wax, J. & Wilson, E. 2004. ‘The risks of underwater birth’, American Journal of Obstetrics and Gynecology 190, 1211-1215.
Royal College of Midwives (RCM). 2013. ‘Campaign for Normal Birth’. Available online at: http://www.rcmnormalbirth.org.uk/about-the-campaign/definitions-and-the-rcm-position-paper
Royal College of Obstetricians and Gynaecologists/Royal College of Midwives (RCOG/RCM). 2006. ‘Immersion in water during labour and birth’. London: Royal College of
Obstetricians and Gynaecologists and Royal College of Midwives.
Russell, K. 2011. ‘Struggling to get into the pool room? a critical discourse analysis of labor ward midwives’ experiences of water birth’, International Journal of Childbirth 1(1), 52-60.
Stark, M.A. & Miller, M.G. 2009. ‘Barriers to the use of hydrotherapy in labor’, Journal of Obstetric, Gynecologic, & Neonatal Nursing 38, 667-675.
Elizabeth Cluett, Ethel Burns
This review includes 12 trials (3243 women).
Water immersion during the first stage of labour significantly reduced epidural/spinal analgesia requirements, without adversely affecting labour duration, operative delivery rates, or neonatal wellbeing.
One trial showed that immersion in water during the second stage of labour increased women’s reported satisfaction with their birth experience.
Further research is needed to assess the effect of immersion in water on neonatal and maternal morbidity.
No trials could be located that assessed the immersion of women in water during the third stage of labour, or evaluating different types of pool/bath.
Background:
Enthusiasts suggest that labouring in water and waterbirth increase maternal relaxation, reduce analgesia requirements and promote a midwifery model of care.
Critics cite the risk of neonatal water inhalation and maternal/neonatal infection.
Objectives:
To assess the evidence from randomised controlled trials about immersion in water during labour and waterbirth on maternal, fetal, neonatal and caregiver outcomes.
Search strategy:
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (30 June 2011) and reference lists of retrieved studies.
Selection criteria:
Randomised controlled trials comparing immersion in any bath tub/pool with no immersion, or other non-pharmacological forms of pain management during labour and/or birth, in women during labour who were considered to be at low risk of complications, as defined by the researchers.
Health topics:
Pregnancy & childbirth > Care during childbirth > Normal labour & birth Pregnancy & childbirth > Care during childbirth > Routine intrapartum care
Data collection and analysis:
We assessed trial eligibility and quality and extracted data independently. One review author entered data and the other checked for accuracy.
Main results:
This review includes 12 trials (3243 women): eight related to just the first stage of labour: one to early versus late immersion in the first stage of labour; two to the first and second stages; and another to the second stage only.
We identified no trials evaluating different baths/pools, or the management of third stage of labour.
Results for the first stage of labour showed there was a significant reduction in the epidural/spinal/paracervical analgesia/anaesthesia rate amongst women allocated to water immersion compared to controls (478/1254 versus 529/1245; risk ratio (RR) 0.90; 95% confidence interval (CI) 0.82 to 0.99, six trials).
There was also a reduction in duration of the first stage of labour (mean difference -32.4 minutes; 95% CI -58.7 to -6.13).
There was no difference in assisted vaginal deliveries (RR 0.86; 95% CI 0.71 to 1.05, seven trials), caesarean sections (RR 1.21; 95% CI 0.87 to 1.68, eight trials), use of oxytocin infusion (RR 0.64; 95%CI 0.32 to 1.28,five trials), perineal trauma or maternal infection.
There were no differences for Apgar score less than seven at five minutes (RR 1.58; 95% CI 0.63 to 3.93, five trials), neonatal unit admissions (RR 1.06; 95% CI 0.71 to 1.57, three trials), or neonatal infection rates (RR 2.00; 95% CI 0.50 to 7.94, five trials).
Of the three trials that compared water immersion during the second stage with no immersion, one trial showed a significantly higher level of satisfaction with the birth experience (RR 0.24; 95% CI 0.07 to 0.80).
A lack of data for some comparisons prevented robust conclusions.
Further research is needed.
Authors’ conclusions:
Evidence suggests that water immersion during the first stage of labour reduces the use of epidural/spinal analgesia and duration of the first stage of labour.
There is limited information for other outcomes related to water use during the first and second stages of labour, due to intervention and outcome variability.
There is no evidence of increased adverse effects to the fetus/neonate or woman from labouring in water or waterbirth.
However, the studies are very variable and considerable heterogeneity was detected for some outcomes.
Further research is needed.
Originally published by Laurie Barclay, MD Medscape Medical News. Jan. 26, 2004
Laboring in water can be helpful in dystocia, according to the results of a randomized controlled trial published online Jan. 26 in the British Medical Journal.
“Incomplete understanding of labour may lead to unnecessarily early intervention,” write Elizabeth R. Cluett, from the University of Southampton in the U.K., and colleagues.
“Labouring in water under midwifery care may be an option for slow progress in labour, reducing the need for obstetric intervention, and offering an alternative pain management strategy.”
To test their hypothesis that laboring in water can relieve pain and anxiety and thereby reduce the need for interventions, the authors compared outcomes for immersion in water in a birth pool during the first stage of labor with those for standard augmentation including amniotomy and intravenous oxytocin.
Subjects were 99 nulliparous women with low risk of complications and with dystocia, defined as cervical dilation rate less than 1 cm/hour in active labor. Primary outcome measures were rates of epidural analgesia and operative delivery.
Compared with women receiving standard care, those receiving water immersion had a lower rate of epidural analgesia (47% vs. 66%; relative risk [RR], 0.71; 95% confidence interval [CI], 0.49 – 1.01), number needed to treat [NNT] for benefit = 5).
Rates of operative delivery (49% vs. 50%; RR, 0.98; 95% CI, 0.65 – 1.47; NNT = 9 and overall labor length were similar in both groups.
However, significantly fewer women in the water immersion group received augmentation (71% vs. 96%; RR, 0.74; 95% CI, 0.59 – 0.88; NNT = 4) or any obstetric interventions including amniotomy, oxytocin, epidural, or operative delivery (80% vs. 98%; RR, 0.81; 95% CI, 0.67 – 0.92; NNT = 5).
Women in the water immersion group also reported significantly lower pain scores and higher satisfaction with freedom of movement than did women in the standard care group.
Although more newborns in the water group were admitted to the neonatal unit (6 vs. 0; P = .013), there was no difference between groups in Apgar score, infection rates, or umbilical cord pH.
Limitations of this study include recruitment of only 99 of 220 eligible women, increased difficulty with recruitment toward the end of the trial because of changes in standard care, and sample size too small to detect statistical differences in use of epidural analgesia.
“Delaying augmentation in association with a supportive environment (water immersion) is acceptable to women with dystocia and may reduce the need for epidural analgesia without increasing labor length or operative deliveries,” the authors write.
“A management approach that reduces rates of augmentation and associated obstetric intervention may contribute positively to maternal physiological and psychological health: oxytocin infusion is known to increase the risk of uterine hyperstimulation and fetal hypoxia, and obstetric interventions are associated with lower maternal satisfaction.”
The authors report no financial conflicts of interest. BMJ. Published online Jan. 26, 2004. Reviewed by Gary D. Vogin, MD
Australian College of Midwives – 2013
This position statement should be read in conjunction with the Australian College of Midwives’ (ACM) position statement for midwives caring for women who make choices outside professional advice.
The ACM supports the choice of women to have the opportunity to access water immersion for labour and/or birth. The ACM identifies six key principles for the safe use of water immersion for labour and birth.
Key principles
1. Warm water immersion has been used for relieving the intensity of pain associated with labour. Warm water and buoyancy elevates the release of endorphins and facilitates relaxation.
2. There are many benefits of using immersion in water during labour, including increasing women’s feelings of control and satisfaction, less painful contractions and less need for pharmacological analgesia, shorter labour, less need for augmentation, with no known adverse effects for the woman herself.
3. Women should be provided with unbiased evidence-based information during pregnancy about their options for labour and birth, including water immersion in labour and/or birth, in order to make informed choices.
4. Informed decision-making, informed consent, and right of refusal are accepted principles in Australia. Each and every woman has the right to make informed decisions, including consent or refusal of any aspect of her care. Women must be respected in the choices that they make.
5. Midwives have a primary responsibility to ensure that their decisions, recommendations and practices are focused on the needs and safety of the woman and her baby/babies.
6. There is no evidence of significant increases in perinatal mortality or morbidity although there are some reports of rare complications. There is limited research on the safety of birth in water and most of the evidence that does exist, is restricted to healthy women with uncomplicated pregnancies.
Achieving best practice
To achieve best practice in the use of water immersion for labour and birth, it is necessary for consumers, professional colleges, education providers, health systems, Australian and State and Territory governments and policy makers to work together to:
Resources to guide practice
The ACM recommends the use of the following resources to guide midwives in their practice:
Date of Issue; 30th May 2013
Date of Review; 29th May 2016
Immersion in water for pain relief and the risk of intrapartum transfer among low risk nulliparous women: secondary analysis of the Birthplace national prospective cohort study
Mirjam Lukasse, Rachel Rowe, John Townend, Marian Knight and Jennifer Hollowell
Abstract
Background: Immersion in water during labour is an important non-pharmacological method to manage labour pain, particularly in midwifery-led care settings where pharmacological methods are limited.
This study investigates the association between immersion for pain relief and transfer before birth and other maternal outcomes.
Methods:
A prospective cohort study of 16,577 low risk nulliparous women planning birth at home, in a freestanding midwifery unit (FMU) or in an alongside midwifery unit (AMU) in England between April 2008 and April 2010.
Results:
Immersion in water for pain relief was common; 50% in planned home births, 54% in FMUs and 38% in AMUs.
Immersion in water was associated with a lower risk of transfer before birth for births planned at home (adjusted RR 0.88; 95% CI 0.79–0.99), in FMUs (adjusted RR 0.59; 95% CI 0.50–0.70) and in AMUs (adjusted RR 0.78; 95% CI 0.69–0.88).
For births planned in FMUs, immersion in water was associated with a lower risk of intrapartum caesarean section (RR 0.61; 95% CI 0.44–0.84) and a higher chance of a straightforward vaginal birth (RR 1.09; 95% CI 1.04–1.15).
These beneficial effects were not seen in births planned at home or AMUs.
Conclusions:
Immersion of water for pain relief was associated with a significant reduction in risk of transfer before birth for nulliparous women.
Overall, immersion in water was associated with fewer interventions during labour.
The effect varied across birth settings with least effect in planned home births and a larger effect observed for planned FMU births.
Full article is available to read via the link below and is highly recommended, with some very detailed analysis and insight into methods of study with statistical support.
Please click here to read the full publication

The New Zealand College of Midwives (Inc) supports immersion of women in warm water during labour as a method of pain management.
Guidelines:
Midwives offering water immersion for labour and for birth are responsible for ensuring the information given to women is accurate and up to date. The following guidelines are recommended:
References:
Title: Labour and delivery in the birthing pool
Author: Forde, C, Creighton, S, Batty, A, Howden, J, Summers-Ma, S, and Ridgeway, G
Title: Warm tub bathing during labour: maternal and neonatal effects
Authors: Ohlsson, G, Buchave, P, Leandersson, U, Nordstrom, L, Rydhstrom, H, and Sjolin, I
Source: Acta Obstetricia et Gynecologica Scandinavica, Vol 80, pp 311 – 314, 2001
Title: Immersion in water in the first stage of labour: a randomised controlled trial Authors: Eckert, K, Turnbull, D, and MacLennan, A
Source: Birth, Volume 28, No 2, pp 84–93, June 2001
Title: Immersion in water during first stage of labour
Author: Homer, C
Source: Letter to the editor, Birth, Vol. 29, No 1, March, 2002
Title: Waterbirths: a comparative study. A prospective study on more than 2000 waterbirths
Authors: Geissbuhler, V and Eberhard, J
Source: Foetal Diagnosis Therapy, Vol. 15, pp. 291 – 300, 2000
Title: Immersion in water in pregnancy, labour and birth
Author: Nikodem, VC
Source: Cochrane Database Systematic Review, 2000
Title: Perinatal mortality and morbidity among babies delivered in water: surveillance study and postal survey
Authors: Gilbert, R and Tookey, P
Source: British Medical Journal, 319 (7208), pp. 483 – 487, 1999
Title: Birth under water – to breathe or not to breath
Author: Johnson, P
Source: British Journal of Obstetrics and Gynaecology, 103, 202-208, 1996
Title: Labour and birth in water: temperature of pool is important
Authors: Deans, AC and Steer, PJ
Source: British Medical Journal. 311:390-391, 1995
Title: Waterbirth – An attitude to care
Author: Garland, D
Source: Books for Midwives, 1995. Chesire
Title: Foetal hypothermia risk from warm water immersion
Author: Charles, C
Source: British Journal of Midwifery

Judy Slome Cohain
originally published December 2010
Abstract: A single case of early onset newborn Group B Strep was documented among 4,432 hospital births into water in the absence of GBS prophylaxis, suggesting that low risk women giving birth into water have a 300% lower rate of newborn GBS disease newborns than dry, full term births delivered by current GBS guidelines.
Possible explanations include:
1) Inoculating the baby with mother’s intestinal flora at birth protects against GBS infection;
2) Bath water washes off the GBS bacteria acquired during the descent through the vagina;
3) Pool dilutes the GBS among a multitude of other intestinal bacteria which compete with GBS;
4) Early onset GBS disease is prevented by lower level of interventions at water birth which promotes maternal and fetal immune function;
5) Kangaroo care after water birth promotes immune function of mother newborn dyad. Much is still to be learned from research documenting birth into water.
Group B Strep (GBS) inhabits the intestines.
Some minutes before the time of birth, the descending fetal head usually causes fecal matter to be excreted. If the woman is in water, the feces enters the water.
A bathtub can be quickly emptied before the fetal head is born.
If she is in a pool, the warm water is likely to be inoculated with GBS. Warm wet conditions enhance the reproduction of bacteria, increasing their numbers exponentially every few minutes.
If the baby’s is born into the warm, feces-exposed water, the baby is exposed to the mother’s intestinal bacteria.
Exposing the baby to the mother’s own natural flora is known to be one of many protective processes that are meant to take place immediately after birth.
Even so, birthing a baby into a feces soiled pool may be considered by many to be likely to increase the risk of newborn infection.
However, evidence of adverse outcomes is lacking.
A report of 4,030 births into water reports no deaths from early onset GBS and one GBS infection.
(1) Information is lacking as to whether the reported GBS-infected baby may also have had a chromosomal abnormality and/or increased blood loss from a snapped umbilical cord or shoulder dystocia.
When this study was conducted, the full term dry birth rate for GBS disease was six times higher (1 in 588) than the waterbirth GBS rate.
The current full term dry birth GBS rate is three times higher (1 in 1,450) than the reported waterbirth rate.(3)
The Cochrane review (2) includes three additional studies tallying another 402 women who birthed their babies into water for which no cases of newborn GBS infection occurred.
The full term waterbirth GBS rate is therefore, a fraction of the dry birth GBS infection rate even after implementation of the US Center for Disease Control (CDC) protocols.
The rate of early onset GBS disease among newborns born before 37 weeks gestation was 1 in 330(3).
Unfortunately research is lacking for whether this rate could also be lowered by birthing into water.
The 2010 CDC Guidelines (5) begins with the statement : “Maternal intrapartum GBS colonization is the primary risk factor for early-onset disease in infants.”
This statement is derived solely from data from interventive land birth, therefore making an incorrect assumption that all births take place in interventive hospital environments.
The evidence regarding GBS and waterbirth is missing from the CDC Guidelines. Objecting to the hospital waterbirth data on the basis of it not being randomized or a small sample is negated by the fact that there are no RCT trials supporting CDC Guidelines(4) and the largest samples included in the new CDC protocols are nonrandomized samples of 5,000 and 7,600 used to
1
support the low rate of anaphylaxis in women given prophylactic antibiotics. ( 5 )
The CDC(5) states definitively that “GBS also can invade through intact membranes (32,33)”.
The words ‘invade through intact membranes’ explicitly describes GBS making a hole rather than a blood borne mechanism.
This statement contradicts a later statement in the same protocols that early newborn GBS infection following elective CS in the presence of intact membranes is either completely or almost non-existant.
The only references supporting GBS ‘invading thru intact membranes’ are from 1984(6) and 1988(7) and do not refer to full term birth.
The first reports on 15 births less than 1000 g, before 28 weeks and all suffering from symptomatic intrauterine infections before birth.
The second reference states: “10-50% of group B streptococcal infections occur in the presence of intact membranes” which is a wild supposition not supported by any other research.
A mechanism is lacking for how GBS might have crossed both the amnion’s and chorion’s thick cross-linkages in the collagen triple helix that provide strength to the collagen.
The compact fibroblast layers of connective tissue beneath the basement membrane form a fibrous barrier. Interstitial collagens predominate and form parallel bundles of collagen fibrils that maintain the mechanical integrity of the amnion.
As an experienced practitioner knows, even with the aid of a sharp amniohook, it can be challenging to break thru two layers of healthy membranes without the presence of a bulging bag of water.
A close examination of CDC guidelines brings into question why certain dubious research is included and other research missing.
While birthing into water may appear counterintuitive, evidence strongly suggests that it protects babies from GBS disease.
Five possible mechanisms for how water birth may protect against GBS disease are suggested in the abstract.
While infusing women with high doses of IV antibiotics to suppress the GBS before the baby passes through, has been widely accepted as current protocol, the Cochrane review emphasizes the lack of RCT studies and the high risk of bias in the 3 small studies that exist. (4)
Routine antibiotic prophylaxis makes light of the biological adaptive abilities of bacteria.
Bacteria have developed many intriguing mechanisms like selectively pumping antibiotics out of their bodies and even digesting antibiotics for nutrition.(8)
The microorganism producing the antibiotic, must have a mechanism to keep itself unharmed by the antibiotic it produces.
Therefore, perfect antibiotic ‘resistance’, a euphemism for immunity, exists before the antibiotic is created.
GBS disease is increasing.
The overall incidence of early onset GBS disease of the newborn showed an initial downward trend from 2000 to 2003 (0.52 to 0.31 cases per 1,000 live births) followed by an increase from 2003 to 2006 (0.31 to 0.40 cases per 1,000 live birth.(9)
Not only is early onset GBS increasing but late onset GBS which is immune to prophylaxis is also increasing above previous levels (2003–2005).(9)
Finally, adult GBS has increased by 32% and it is predicted that this rate will continue to increase.(9)
Seven percent of adults are allergic to penicillin and therefore already have no effective treatment for the 20% of GBS that is erythromycin- and clindamycin- resistant(4).
In addition, a new disease that causes painful vaginal burning sensation without relief for years, called long-term symptomatic GBS vaginitis, first described in case studies in 1997, is now becoming more and more common and likely involves antibiotic resistant strains of GBS, since antibiotics are not consistently useful to eradicate it.(10)
Hospital Birth into Water data appears to provide the lowest Newborn GBS disease outcomes available without increasing the dangers of antibiotic resistance.
References:
1. Gilbert R.E. and P.A. Tookey. 1999. Perinatal mortality and morbidity among babies delivered in water: surveillance study and postal survey. BMJ 319: 483–87.
2. Cluett, E.R. and E. Burns. 2009. Immersion in water in labour and birth. Cochrane Database of Systematic Reviews (2) DOI: 10.1002/14651858.CD000111.pub3.
3. Phares C.R., et al. 2009. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. JAMA 299(17): 2056–65.
4. Ohlsson A, Shah VS. Intrapartum antibiotics for known maternal Group B streptococcal colonization. Cochrane Databaseof Systematic Reviews 2009, Issue 3. Art. No.: CD007467.
5. Prevention of Perinatal Group B Streptococcal Disease. Revised Guidelines from CDC. 2010. November 19, 2010/59(RR10);1-32.
6. Desa DJ, Trevenen CL. Intrauterine infections with group B beta-haemolytic streptococci. Br J Obstet Gynaecol 1984;91:237–9.
7. Katz V, Bowes WA Jr. Perinatal group B streptococcal infections across intact amniotic membranes. J Reprod Med 1988;33:445–9.
8.http://www.scientificamerican.com/podcast/episode.cfm?id=166B51F8-DE9C-DCF8- 9132AF8A95CA0642 Accessed 1 Sept 2010.
9. Centers for Disease Control and Prevention. 2009. Trends in perinatal group B streptococcal disease — United States, 2000–2006. MMWR Morb Mortal Wkly Rep 58(5): 109–12.
10. Cohain, J.S. 2009. Long term Symptomatic GBS Vulvovaginitis — eight cases resolved with freshly cut garlic. Eur J Obstet Gynecol Reprod Biol 146(1): 110–11.

20 November 2015:
Since the early 1980s use of immersion in water during labour and birth has been increasingly promoted to enable women to relax, help them cope with pain, and maximise their feelings of control and satisfaction1-4.
In 1992 the House of Commons Health Committee recommended all hospitals provide the option of a birthing pool where practicable5. Currently few women give birth in water but the option of immersion or showering during the first stage of labour is commonly available.6-8
Although problems have arise which have been attributed to water use, the results of the most formal evaluations have not clearly associated water use with harmful outcomes for mother or baby 3,9-13.
The lack of robust evidence of harm or benefit means that childbearing women and health practitioners alike are subject to conflicting opinion about the usefulness and safest of water, particularly for birth.
However, a recent observational study over a nine year period concluded that ‘waterbirth was associated with low risks where obstetric guidelines were followed’16.
At present in the UK there is no reliable measurement of the rate of birth in water. A national survey of maternity units in the UK in 2002 found that 63% (216/342) had a birthing pool8; 67% (228/342) reported having at least one midwife trained to provide support for women giving birth in water and 36% (121/342) said that at least half of the midwives working in their unit were trained to support birth in water.
How is water used during labour?
Water use ranges from informal, for example when a woman in early labour decides to get into her bath at home before going to hospital, to formal use in a specially designed birthing pool. Informal use in a domestic bath or shower is often initiated by a woman herself to help her cope at home before her labour is well established.
Formal use implies either that a woman has actively chosen to use water as part of her plan for labour and/or childbirth or that a health professional, usually a midwife, has suggested use during established labour.
Why water use is promoted
Use of immersion in water during childbirth has largely been driven by pregnant and birthing women17 and supported by midwives. During the first stage of labour it is advocated to shorten labour and help a woman relax and cope with contractions, feel more in control, and to reduce intervention by health professionals3,18-21.
During the second stage, proponents use it to allow perineal tissues to stretch spontaneously, birth to occur with minimum intervention, and to provide the baby with a gentler transition into extra-uterine life. Expectant management of the third stage is likely if a woman is in water.
Limitations on water use
Many health professionals consider that water use during the first stage of labour in uncomplicated pregnancy is unlikely to harm the mother or baby22,23, whilst others have concerns about water use at any point in labour14.
Local clinical guidelines may restrict water use to women considered at ‘low’ obstetric risk7, and other aspects of care may be prescribed, for example when and how to monitor the temperature of the water, the degree of cervical dilatation at which to begin its use24, and whether the immersion is considered safe for all stages of labour6,25.
Problems associated with possible risk of infection or cross infection caused by amniotic fluid, blood, and faeces have been described26-28 and some hospitals have restricted use of birthing pools to women who have tested HIV negative during pregnancy29.
However, at a multi-disciplinary consensus meeting held in London in 1996, it was agreed that mandatory HIV testing for prospective users of birthing pools could be an extreme reaction to the perceived risks and that high standards of pool hygiene would be an appropriate way forward30. Local infection control guidelines should cover the use of water pools25,31 and procedures to minimise risk of cross infection13, 32.
It has been suggested that high water temperature can cause serious changes in feto-maternal haemodynamic regulation and fetal thermoregulation33. It has been reported that fetal tachycardia can be reduced by cooling the water34 and most providers and clinical guidelines specify a temperature range within which the water should be maintained during the first and second stage of labour7,35.
The prospect of a woman giving birth in water can cause anxiety about how to deal with unexpected emergencies such as shoulder dystocia, the need to avoid the baby inhaling water, or being unaware that the umbilical cord has been severed11.
Despite the fact that it denies women choice about birth, one response has been to limit water use to first stage only6. Development of agreed clinical protocols to deal with unexpected complications25 and providing training which allows3 staff to achieve relevant competencies is key to enabling real choice for women about use of water.
There are theoretical risks of increased blood loss, retained placenta, or water embolism, and professional advice is often to conduct the third stage out of water25.
Because water adds to the difficulty of estimating blood loss accurately, it has been proposed that blood loss would be more appropriately estimated as being either more or less than 500ml36 and that the overall physical condition of the woman should be used as the most important indicator to assess the impact of any bleeding37.
In summary, although not universally accepted, first stage water use is less controversial than immersion for the second or third stage of labour22,23,38.
The research evidence
The effects of water use during the first stage of labour on maternal and fetal outcomes have been evaluated in several randomised controlled trials4,9,10,12,13,39 with sample sizes ranging from 60 to 123934.
The use of water has been shown to reduce the rate of augmentation40; however, no trial has been large enough to measure the effect of water use on important neonatal outcomes such as perinatal death or other serious neonatal or maternal morbidity.
In addition, there has often been significant cross-over between study groups4,12, reducing the likelihood of identifying clear differences between women allocated to water use and those not.
A systematic review of eight trials41 indicated a statistically significant reduction in the use of pain relief with no such significant difference in the rate of operative deliveries or in neonatal outcomes.
It concluded that while the use of water in the first stage of labour can be of benefit to some women, there is no evidence at present to support or not support a woman’s choice to give birth in water.
Retrospective comparison has been made of women who have used water with those who have not42,43.
However, there are considerable difficulties in interpreting such studies because of the possibility that the results are inherently biased.
In the same way, findings of cohort studies which suggest benefit for water use in terms of pain relief and increased rate of cervical dilatation44-47, or those which indicate differences in rates of maternal and neonatal infection48-50, are also open to criticism.
A recent study16 compared neonatal and maternal morbidity and mortality for spontaneous singleton births that took place in water or on land.
This was an observational study over a nine year period and data were obtained through standardised questionnaires for 9,518 births, of which 3,617 were waterbirths and 5,901 landbirths.
Statistically significant differences were identified between the two groups; women who gave birth using water were less likely to suffer serious perineal trauma, use no analgesia and have a lower blood loss than women in the landbirth group.
Maternal and neonatal infection rates were the same for both groups, but more landbirth babies had neonatal complications requiring transfer to an external NICU.
During the study, there were neither maternal nor neonatal deaths related to spontaneous labor.
The authors acknowledge the potential bias that could arise from the self-selection issue but argue that this is well accounted for in the analysis.They conclude that waterbirths are associated with low risks for both mother and child when obstetrical guidelines are followed.
Another study51 based in a centre for low risk women was a retrospective case review over a five year period of 1355 births in water.
When compared with land births over a corresponding period, women who gave birth in water had significantly fewer episiotomies with no evidence of a corresponding rise in lacerations, a reduction in the length of the first stage of labour, no increase in the risk of acquired infection or aspiration pneumonia and considerably lower levels of analgesia use.
Neonatal condition assessed by arterial cord blood pH, base excess and birth weight showed no differences.The authors conclude that this represents a realistic option for women at low risk of complications.
Many reports about water use are case series1,20,52-62 and focus on perceived benefits of water use for the mother, her baby and birth attendant.
These include shorter labour52, less use of pharmacological analgesics46,53, less intervention by care givers19, lower rate of perineal trauma60-62, and increased satisfaction with the experience of labour and birth54.
By contrast, some case reports have highlighted serious problems such as fetal overheating33,34, neonatal sepsis28, near drowning63 or death64.
Overall, reviews of the evidence21,23,65,66 conclude that appropriately large-scale research is still required to evaluate rigorously the physiological effects13, clinical outcomes, and economic impact of water use.
What we don’t know
The current evidence about water use remains quite heavily dependent on case series and comparison studies that include varying sized samples.
Therefore, reliable evidence about efficacy and effectiveness is still equivocal67.
Implications for maternity
Water use during the first stage of labour is offered by the majority of maternity care provider units in the UK and most offer support for water birth8.
Introduction of, and sustained suppor t for, water use may have considerable implications for service governance68.
However, not all costs fall to providers of care; a substantial cost burden is likely to be borne by labouring women themselves during informal use in domestic baths and showers or by hiring specially designed pools for use in their home or in a maternity unit.
Most maternity units have installed a water pool for use in labour8 and although installation and maintenance of a specially designed pool in a maternity unit involves obvious financial cost, this may be offset if there is a reduction in analgesia and anaesthetic use44.
There is evidence that formal water use means that at least one midwife will be in constant attendance during the first stage of labour and that at least two will be in attendance for birth7.
This level of staffing may be difficult to sustain and may have implications for equity of care for women who do not use water22.
Clear strategies for the training, preparation and support of staff who offer use of water during labour are recognised as essential7,25,31,37,44.
Key components of these include clarification of the roles of different maternity health professionals, multi-disciplinary development of local protocols, development of guidelines for clinical practice, and short-term secondment of midwives to learn alongside practitioners skilled and experienced in water use.
Implications for practice
Women may choose to use immersion in water during labour and/or birth. Midwives and other maternity care workers should therefore be knowledgeable about the evidence in terms of potential advantages and disadvantages.
Given the current quality of reliable evidence, effective practice is likely to be informed and influenced substantially by shared experience and personal observation.
Disproportionate weight may therefore be placed on perceived disadvantages or advantages and credibility given to outcomes which may not be associated causally with water use.
Practitioners should be alert to the evolving evidence base which underpins the use of water.
Reproduced from Midirs 2005, last revised Jan 2005, review date Jan 2007. Informed Choice is supported by the Royal College of Midwives and the National Childbirth Trust.
References
8 December 2015:
Rowena Davies, RM, BA 1, 2
Deborah Davis RM, PhD1, 2
Melissa Pearce RM/RN, BNurs, GDipMid, GCertMid, MMidwifery2, 3
Nola Wong, RM/RN2, 3
1. Nursing and Midwifery, Faculty of Health, University of Canberra
2. The Australian Capital Regional Centre for Evidence Based Nursing and Midwifery Practice: an affiliate centre of the Joanna Briggs Institute
3. Centenary Hospital for Women and Children, Canberra
Corresponding author:
Rowena Davies
u3053358@uni.canberra.edu.au
The objective of this research is to systematically review the evidence regarding the effect of waterbirth, in comparison to land birth, on the mortality and morbidity of neonates born to low risk women.
Waterbirth and water immersion in labor are two distinct phenomena; however they are often confounded. Some women use water immersion in labor as a strategy to manage their labor pain but leave the bath prior to the birth of their baby.
As the name implies, however, waterbirth occurs when a baby is born underwater. This can happen either intentionally or accidentally, for example when a woman uses water immersion during labor and remains in the water to birth her baby.
Although the definitions of waterbirth and water immersion are simple to separate, descriptions of their use during a woman’s labor are often merged. 1,2
Given this, it is not surprising that research attempting to describe the benefits and risks of both water immersion and waterbirth is interwoven.
In many instances, discussion of waterbirth is confused by focusing on the benefits of water immersion for the woman and the risks of waterbirth to the neonate, two separate issues.
Water immersion in labor
Water immersion in labor has been used by many generations of women and is common practice in many birthing suites.3 Current research describes benefits for women using water immersion in labor including: increased relaxation4, pain relief5,6, maximized maternal satisfaction7, reduced length of labor2,3,5,8,9, reduced intervention3,10,11, increased spontaneous birth 12,13 and reduced first and second degree perineal tears.13,14
The buoyancy enabled by the water allows women to move easier during labor and potentially optimizes labor progress.3,6 Water immersion may also be associated with improved uterine perfusion, less painful contractions and a shorter labor.3,15,16
A Cochrane systematic review of eight trials comparing water immersion in labor with controls showed that water immersion resulted in a significant reduction in epidural analgesia use (478/1254 versus 529/1245; risk ratio [RR] 0.90; 95% [Confidence Interval [CI] 0.82 to 0.99, six trials]), a reduction in duration of the first stage of labor (mean difference -32.4 minutes; 95% CI -58.7 to -6.13, seven trials) with no difference in assisted vaginal birth (RR 0.86; 95% CI 0.71 to 1.05, seven trials), caesarean sections (RR 1.21; 95% CI 0.87 to 1.68, eight trials), use of oxytocin infusion (RR 0.64; 95%CI 0.32 to 1.28, five trials), perineal trauma (intact perineum, 236/678 versus 200/659, RR 1.16, 95% CI 0.99 to 1.35, five trials) or maternal infection (15/647 versus 15/648, RR 0.99, 95% CI 0.50 to 1.96, five trials). 5 There have been no studies that have identified any adverse effects of water immersion in labor for the woman or the neonate.
Waterbirth
The benefits to women of using water immersion in labor are evident. However, the practice of birth underwater remains controversial and the debate polarized, with research providing conflicting information and mixed results.
As a result of this confusion, many birthing units in Australia provide water immersion in labor as an option for women; however, implementing waterbirth policies remains a slow and complex process.17,18
The trend of waterbirth
The first recorded waterbirth occurred in France in 1803.19 After laboring for 48 hours, an exhausted woman used a warm bath and birthed a healthy baby.1 In the early 1980s, waterbirths became more popular as water immersion was promoted to help women relax and cope with their labor.20, 21
Currently, few women birth their baby underwater; however water immersion in labor is commonly available.20 Baths and birthing pools were integrated into the United Kingdom’s mainstream maternity units in 1992 after the House of Commons Health Committee recommended that all women have access to water for labor and birth.12
Their national practice guidelines also support the use of baths and birthing pools in labor.22 Within Australia, 14 of 19 birthing centres provide bath facilities.23 Further, waterbirth tends to be supported by midwives as it represents a birthing option congruent with midwifery philosophy.7,24
Concerns about waterbirth
In an uncomplicated pregnancy, water immersion is unlikely to harm the woman or her baby.5 Given this, many birthing units will restrict water immersion in labor to women with a low risk pregnancy.
Regarding waterbirth, commentators have developed a list of contraindications; however, due to a paucity of research in this area, this is based largely on opinion.18 Even so, the option to waterbirth remains restricted to women with a low risk pregnancy. Individual birthing units develop specific waterbirth protocols suiting their own circumstances and existing policy.
In a review of the evidence on waterbirth, Young and Kruske (2013) identified five main areas of concern: a perceived risk of neonatal water aspiration, neonatal and maternal infection, neonatal and maternal thermo-regulation, skills of attending midwives and emergency procedures in the event of maternal collapse. They concluded there was no evidence supporting these concerns.25
Although the practice of waterbirth has been linked to increased risk to the neonate1, 26-28 there is no high level evidence available to support this issue.20,29 The association between waterbirth and adverse neonatal outcomes comes largely from case reports. 28,30,31
These highlight the potential risks to the neonate from waterbirth, including: neonatal respiratory distress, neonatal infection, umbilical cord avulsion, hyponatremia, hypoxic ischemic encephalopathy, fetal thermoregulation and water embolism.1,26,28,32,33
There are also numerous articles providing commentary about a perceived lack of adequate research and potential disregard for adverse neonatal outcomes following waterbirth.18,32, 34-36 Both case studies and commentary are at risk of author bias and represent a low level of evidence upon which to build waterbirth policy and protocol.
The above neonatal outcomes, as described within the literature, will form the basis of the reviewers search and discussion concerning potential neonatal outcomes following waterbirth.
Current evidence and policy
Simpson (2013)37 conducted a systematic review of neonatal outcomes following waterbirth; however, only two randomized controlled trials (RCT), two systematic reviews and case reports were reviewed.
A number of observational studies have been conducted on waterbirth but these were not included.37Also, no meta-analysis was conducted. The Cochrane systematic review by Cluett and Burns (2009) was similarly limited to RCTs. 5 Another systematic review, conducted in 2004, searched for complications that could be associated with waterbirth and was not limited to RCTs.1
They reviewed 16 articles and concluded that waterbirth may be associated with complications that are not seen with land birth, however, outcomes from water immersion and waterbirth are confounded.1 The quality and rigor of this review has also been called into question.35
There are two known RCTs comparing outcomes after waterbirth and land birth: an Iranian study of 106 women38 and a pilot study conducted in the UK.29 Both trials are small and therefore offer limited evidence. Woodward and Kelly (2009) reported that a larger RCT is possible and acceptable to women; however no further trial has been conducted hence raising concerns over feasibility.29
Published guidelines for health practitioners argue that there is insufficient evidence to guide waterbirth practice. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists offer a cautious review, suggesting that there is little evidence of waterbirth offering any benefits and advise caution when interpreting any current studies due to small sample sizes.39
The American College of Obstetricians and Gynecologists (2014) state that waterbirth “should be considered an experimental procedure that should only be performed within the context of an appropriately designed clinical trial with informed consent”40(p.914). However, it is unlikely that a RCT could ethically be conducted on this practice.
Other protocols agree that there may be no benefit, but argue that there is also no adverse effects directly attributed to waterbirth. A joint statement released by the Royal College of Obstetrics and Gynaecology (RCOG) and the Royal College of Midwives (RCM) support women laboring in water while acknowledging the lack of evidence supporting waterbirth and the rarity of complications.41
The Queensland Normal Birth guidelines also discuss waterbirth stating there is no evidence of increased adverse effects for the woman or fetus; however they acknowledge there is inadequate evidence to either support or not support, a woman’s choice to birth underwater.42
Young and Kruske (2012) confirm that Australia’s individual state policies lack contemporary, high quality evidence and do not encourage or provide guidance for women or their health care providers. 43
The current state of opinion and evidence of the benefits and risks of waterbirth for the neonate requires a thorough systematic review to be conducted. Current evidence is contradictory and the lack of robust systematic evidence regarding waterbirth allows the growth of conflicting opinion about its safety.
Given the scarcity of reliable evidence, anecdotal shared experiences and personal observation has influenced policy and practice. 20 A review of current literature focusing on high level evidence and maintaining clear and thorough search guidelines is needed to advance our understanding of the effect of waterbirth on neonatal outcomes.
Waterbirth; neonatal outcomes; mortality; morbidity
Inclusion criteria
This review will consider studies that include low risk, healthy, pregnant women who labor and birth spontaneously, at term (37-42 weeks), with a single baby in a cephalic presentation.
Low risk pregnancies are defined as pregnancies with an absence of comorbidity or obstetric complication, such as maternal diabetes, previous caesarean section birth, high blood pressure or other illness. Women may be experiencing their first or subsequent pregnancy. The baby must also be well and without any comorbidity or complication.
Types of intervention(s)/phenomena of interest
The intervention of interest is waterbirth. The comparator is land birth. Women and their babies must be cared for by qualified maternity healthcare providers throughout their labor and birth. The birth setting must be clearly described but can include homebirth, hospital birth or birth center, either freestanding or attached to a hospital.
This review will consider studies that include the following neonatal outcome measures:
1. Neonatal mortality- stillbirth or neonatal death within 28 days of birth
2. Neonatal resuscitation or Respiratory Distress Syndrome within 24 hours of birth
3. Neonatal sepsis/infection, including fever and other infection markers, as defined within any studies, within seven days of birth
4. APGAR scores at one, five and ten minutes
5. Admission to Neonatal Intensive Care Unit or Special Care Nursery, including length of stay
6. Cord pH values – arterial and/or venous taken immediately following birth
7. Cord avulsion
8. Hyponatremia
9. Hypoxic ischemic encephalopathy
10. Birth injury
This review will consider studies that compare neonatal outcomes for both waterbirth and land birth including randomized controlled trials, quasi-experimental studies, prospective and retrospective cohort studies. Descriptive studies that do not include a comparator will be excluded.
The search strategy aims to find both published and unpublished studies. A three step search strategy will be utilized in this review. An initial search of MEDLINE and CINAHL will be undertaken followed by an analysis of the text words contained in the title and abstract, and of the index terms used to describe the article.
A second search using all identified keywords and index terms will then be undertaken across all included databases. Thirdly, the reference lists of all identified reports and articles will be searched for additional studies.
Studies published in English within the last 15 years (from 1999) will be considered for inclusion. This ensures that retrieved studies will provide recent, up-to-date evidence that will reflect more contemporary practice and policy.
References
| 1. Pinette MG, Wax J, Wilson E. The risks of underwater birth. Am J Obstet Gynecol.2004; 190(5): 1211-5.
http://dx.doi.org/10.1016/j.ajog.2003.12.007 PMid:15167820 |
|||
| 2. Thoeni A, Zech N, Moroder L, Ploner F. Review of 1600 water births. Does water birth increase the risk of neonatal infection. J Matern Fetal Neonatal Med.2005; 17(5): 357-61.
http://dx.doi.org/10.1080/14767050500140388 PMid:16147851 |
|||
| 3. Otigbah CH, Dhanjal MK, Harmsworth G, Chard T. A retrospective comparison of water births and conventional vaginal deliveries. Eur J Obstet Gynecol Reprod Biol.2000; 91(1): 15-20. | |||
| 4. Maude R, Foureur M. It’s beyond water: stories of women’s experience of using water for labour and birth. Women Birth.2007; 20(1): 17-24.
http://dx.doi.org/10.1016/j.wombi.2006.10.005 PMid:17174165 |
|||
| 5. Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Database for Systematic Reviews.2009; (2): doi: 10.1002/14651858.CD000111.pub3. | |||
| 6. Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S. Newburn M. Pain management for women in labour: an overview of systematic reviews. Cochrane Database of Systematic Reviews.2012. doi: 10.1002/14651858.CD009234.pub.2. | |||
| 7. Richmond H. Women’s experience of waterbirth. Pract Midwife.2003; 6(3): 26-31.
PMid:12677840 |
|||
| 8. Richmond H. Theories surrounding waterbirth. Pract Midwife.2003; 6(2): 10-3.
PMid:12621866 |
|||
| 9. Cortes E, Basra R, Kelleher CJ. Waterbirth and pelvic floor injury: a retrospective study and postal survey using ICIQ modular long form questionnaires. Euro J Obstet Gynecol Reprod Biol.2011; 155(1): 27-30.
http://dx.doi.org/10.1016/j.ejogrb.2010.11.012 PMid:21185644 |
|||
| 10. Lukasse M, Rowe R, Townend J, Knight M, Hollowell J. Immersion in water for pain relief and the risk of intrapartum transfer among low-risk nulliparous women: secondary analysis of the Birthplace national prospective cohort study. BMC Pregnancy Childbirth.2014; 14(60): doi: 10.1186/1471-2393-14-60. | |||
| 11. Mollamahmutoglu L, Moraloglu O, Ozyer S, Su FA, Karayalcin R, Hancerlioglu N et.al. The effects of immersion in water on labor, birth and newborn and comparison with epidural analgesia and conventional vaginal delivery. J Turk Ger Gynecol Assoc.2012; 13(1): 45-9.
http://dx.doi.org/10.5152/jtgga.2012.03 PMid:24627674 PMCid:PMC3940223 |
|||
| 12. Burns E, Boulton M, Cluett E, Cornelius V, Smith L. Characteristics, interventions, and outcomes of women who used a birthing pool; a prospective observational study. Birth.2012; 39(3): 192-202.
http://dx.doi.org/10.1111/j.1523-536X.2012.00548.x PMid:23281901 |
|||
| 13. Henderson J. Labouring women who used a birthing pool in obstetric units in Italy: prospective observational study. BMC Pregnancy Childbirth.2014; 14(17): doi: 10.1186/1471-2393-14-17. | |||
| 14. Pagano E, De Rota B, Ferrando A, Petrinco M, Merletti F, Gregori D. An economic evaluation of water birth: the cost-effectiveness of mother well-being. J Eval Clin Pract.2010; 16(5): 916-9.
http://dx.doi.org/10.1111/j.1365-2753.2009.01220.x PMid:20590979 |
|||
| 15. Garland D. Waterbirth in the United Kingdom. Midwifery Today Int Midwife.2000; 54(1): 26.
PMid:11189584 |
|||
| 16. Geissbuhler V, Eberhard J. Waterbirths: a comparative study. A prospective study on more than 2,000 waterbirths. Fetal Diagn Ther.2000; 15(5): 291-300.
PMid:10971083 |
|||
| 17. Dahlen HG, Dowling H, Tracy M, Schmied V, Tracy S. Maternal and perinatal outcomes amongst low risk women giving birth in water compared to six birth positions on land. A descriptive cross sectional study in a birth centre over 12 years. Midwifery.2013; 29(1): 759-764.
http://dx.doi.org/10.1016/j.midw.2012.07.002 PMid:22884894 |
|||
| 18. Veltman L, Doherty D. Safety and underwater birth? What every risk manager should know. Journal Healthc Risk Manage.2013; 32(4): 16-24.
http://dx.doi.org/10.1002/jhrm.21106 PMid:23609973 |
|||
| 19. Embry M. Observation sur un accouchement termaine dans le bain. Ann Soc Med Prat Montpellier; 5(1): 13. | |||
| 20. MIDIRS. The use of water during childbirth. MIDIRS.2005; Retrieved from: www.waterbirth.org/assest/documents/MIDIRS%20waterbirth.pdf. Accessed 4.3.14. | |||
| 21. Odent M. Birth under water. Lancet.1982; (2): 1476-7. | |||
| 22. National Institute of Clinical Excellence. Intrapartum Care: care of healthy women and their babies during childbirth. London.2007; NICE. Retrieved from www.nice.org.ul/CGo55. Accessed 6.3.14. | |||
| 23. Laws PJ, Lim C, Tracy S, Sullivan EA. Characteristics and practices of birth centres in Australia. Aust N Z J Obstetr Gynaecol.2009; 49(3): 290-295.
http://dx.doi.org/10.1111/j.1479-828X.2009.01002.x PMid:19566562 |
|||
| 24. Meyer SL, Weible CM, Woeber K. Perceptions and practice of waterbirth: a survey of Georgia midwives. J Midwifery Womens Health.2010; 55(1): 55-9.
http://dx.doi.org/10.1016/j.jmwh.2009.01.008 PMid:20129230 |
|||
| 25. Young K, Kruske, S. How valid are the common concerns raised against water birth? A focused review of the literature. Women Birth.2013; 26(2): 105-9.
http://dx.doi.org/10.1016/j.wombi.2012.10.006 PMid:23182130 |
|||
| 26. Carpenter L, Weston P. Neonatal respiratory consequences from water birth. J Paediatr Child Health.2012; 48(1): 419-423.
http://dx.doi.org/10.1111/j.1440-1754.2011.02241.x PMid:22085259 |
|||
| 27. Gilbert RE, Tookey PA. Perinatal mortality and morbidity among babies delivered in water: surveillance study and postal survey. BMJ.1999; 319(7208): 483-487. | |||
| 28. Kassim Z, Sellars M, Greenough A. Underwater birth and neonatal respiratory distress. BMJ.2005; 330(1): 1071-2.
http://dx.doi.org/10.1136/bmj.330.7499.1071 PMid:15879398 PMCid:PMC557235 |
|||
| 29. Woodward J, Kelly SM. A pilot study for a randomised controlled trial of waterbirth versus land birth. BJOG.2004; 111(6): 537-45.
http://dx.doi.org/10.1111/j.1471-0528.2004.00132.x PMid:15198780 |
|||
| 30. Cohain JS. Waterbirth and GBS. Midwifery Today Int Midwife.2010; (96): 9-10.
PMid:21322437 |
|||
| 31. Schafer R. Umbilical cord avulsion in waterbirth. J Midwifery Womens Health.2014; 59(1): 91-4.
http://dx.doi.org/10.1111/jmwh.12157 PMid:24588881 |
|||
| 32. Davies MW. Water births and the research required to assess the benefits versus the harms. J Paediatr Child Health.2012; 48(9): 726-729.
http://dx.doi.org/10.1111/j.1440-1754.2010.01781.x PMid:20598065 |
|||
| 33. Eckert K, Turnbull D, MacLennan A. Immersion in water in the first stage of labor: a randomised controlled trial. Birth.2001; 28(2): 84-93.
http://dx.doi.org/10.1046/j.1523-536X.2001.00084.x PMid:11380379 |
|||
| 34. Batton DG, Blackmon LR, Adamkin DH, Bell EF, Denson SE, Engle WA. Underwater births. Pediatrics.2005; 115(1): 1413.
PMid:15867054 |
|||
| 35. Keirse M. Challenging Water Birth? How Wet Can It Get? Birth.2005; 32(4): 318-322.
http://dx.doi.org/10.1111/j.0730-7659.2005.00390.x PMid:16336374 |
|||
| 36. Schroeter K. Water births: a naked emperor. Pediatrics.2004; 114(3): 855-8.
http://dx.doi.org/10.1542/peds.2004-0145 PMid:15342864 |
|||
| 37. Simpson KR. Underwater birth. J Obstet Gynecol Neonatal Nurs.2013; 42(5): 588-94.
http://dx.doi.org/10.1111/1552-6909.12235 PMid:24004064 |
|||
| 38. Chaichian S, Akhlaghi A, Rousta F, Safavi M. Experience of water birth delivery in Iran. Arch Iran Med.2009; 12(5): 469-471. | |||
| 39. Royal Australian and New Zealand College of Obstetricians And Gynaecologists. Warm water immersion in labour and birth. College Statement.2011. Retrieved from . www.ranzcog.edu.au/college-statements-guidelines.html#obstetrics. Accessed 24.4.14. | |||
| 40. American College of Obstetricians and Gynecologists. Immersion in water during labour and delivery. Committee opinion No. 594. Obstet Gynecol.2014; 123(4): 912-5.
http://dx.doi.org/10.1097/01.AOG.0000445585.52522.14 PMid:24785637 |
|||
| 41. Royal College of Obstetricians and Gynaecologists and Royal College of Midwives. Immersion in water during labour and birth. Joint Statement.2006. London: Author. | |||
| 42. Queensland Maternity and Neonatal Clinical Guidelines Program. Normal Birth. 2012. Retrieved from www.health.qld.gov.au/qcg/documents.g_normbirth.pdf. Accessed 3.3.14. | |||
| 43. Young K, Kruske S. Water immersion in Queensland. Evidence, Access and Uptake.2012; Queensland Centre for Mothers and Babies: University of Queensland. Retrieved from http://www.qcmb.org.au/media/pdf/Water%20Immersion%20Report.pdf. Accessed 21.5.14. |

18 February 2016: Midwives Alliance
The MANA and CfM Joint Position Statement on Water Immersion During Labor and Birth is a position paper written for a broad audience including midwives and other birthcare professionals, consumers, doulas, childbirth educators, and policy makers.
It is co-authored by the Midwives Alliance of North America and Citizens for Midwifery.
A year of collaborative work has produced a great educational tool that gives concise access to the research and the wisdom of experience that documents the safety, benefits and recommendations for success.
With over 80 citations, including the new study “Maternal & Newborn Outcomes Following Immersion During Waterbirth” by Bovbjerg, Cheyney and Everson, which utilized data from the MANA Statistics project, and research by waterbirth activist Barbara Harper, the position paper is a reference guide to the evidence for the safety of water immersion during labor and birth.
How does the new study using data from the MANA Statistics project help us better understand waterbirth?
The research of Bovbjerg, Cheyney and Everson helps to dispel some of the more publicized concerns about the safety of waterbirth to the baby, including drowning, cord avulsion and respiratory distress.
No deaths in over 6500 water births were attributable to being born under water. There was also no additional risk of maternal infection or hemorrhage.
The MANA Stats study showed that 35% of over 18,000 home and birth center births occurred in water, demonstrating that the midwives contributing to MANA Stats have considerable experience attending and monitoring births in water.
The experience level of the practitioner may be an important factor in the safety of waterbirth.
6,521 waterbirths, including 13 sets of twins, 29 breeches and 327 VBACs, were compared with 10,252 mothers who did not choose waterbirth, making this the largest comparative study on waterbirth to-date.
Additionally, this is the first large waterbirth study of a US population, with its unique healthcare system and demographics.
While the ACOG/AAP Committee Opinion of April, 2014, not recommending water immersion for birth, acknowledged the limitations of the available research on waterbirth, this large US study fills that gap and gives us the best evidence to-date on the safety of birthing in water.
“Maternal & Newborn Outcomes Following Immersion During Waterbirth” by Bovbjerg et al, was published Jan. 20, 2016 in the Journal of Midwifery & Women’s Health.
JMWH has generously agreed to make this research article open access, so midwives, birth workers, and consumers can read it without needing to buy a subscription to the Journal.
What else can we learn from the MANA/CfM Joint Position Statement?
Evidence and experience show us that mothers choose waterbirth for several reasons.
They report feeling more relaxed, in control, able to move more freely, and, notably, relief from pain.
Especially considering the risks of pharmacologic pain management such as epidural and spinal anesthesia, water immersion during labor and birth may be safer for mother and baby.
“In addition, because water immersion facilitates normal physiologic birth it may also be associated with other beneficial health outcomes for mother and baby, including decreased need for intervention during labor and reduced incidence of surgical/instrumental delivery.”
As in all healthcare and birthcare decisions informed consent/refusal and shared decision making with your care provider is key to determining what is best for each family.
The Joint Position Statement can help in these ways:
The practical and professional pearls of wisdom make the Factors that Promote Safety and Success section an invaluable tool when considering and planning a waterbirth and we are pleased to be able to share them with you.
The conclusion:
Many families consider water immersion during labor and birth a valuable option.
Current research and experience show waterbirth to be safe for mothers and babies and may provide benefits to both.
“MANA and CfM support the use of water immersion during labor and birth, and believe it should be made available to birthing families across all settings.
MANA and CfM encourage all care providers to become educated about the safe use of water immersion during labor and birth, and to engage in a shared decision making process when discussing the option of water immersion with their clients.” (quote from the statement)
The authors of the joint position statement are:
Jill Breen, CPM, CLC; Justine Clegg, CPM, LM, MS; Nasima Pfaffl, MA, President CfM; Amy Smith, CPM
Thanks also to the consultants on the statement:
Barbara Harper, RN, CD, CCE; Holly Horan, MA; Jennie Joseph, LM, CPM, CEO of Commonsense Childbirth, Inc.; Indra Lusero, JD, MA; Jeanette McCulloch, IBCLC; Shafia M. Monroe, MPH, DEM, CDT, President and CEO of the International Center for Traditional Childbearing (ICTC).
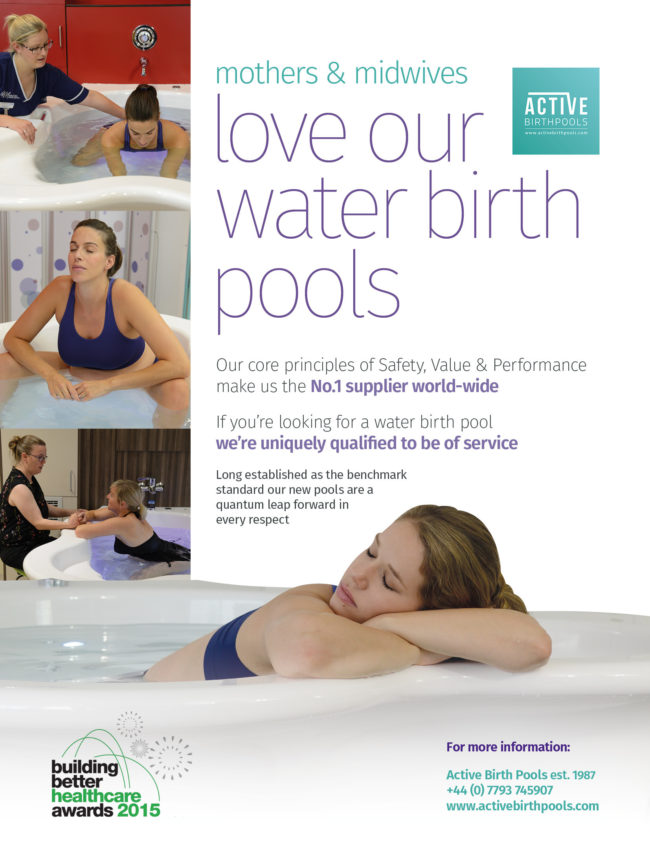
Practice Points
Ensure that pregnant women receive high quality care throughout their pregnancy, have a normal childbirth wherever possible, are involved in decisions about what is best for them and their babies, and have choices about how and where they give birth (DH 2004).
Respect for a woman’s wishes and her involvement in decision making is essential to her care in pregnancy and labour (NICE 2007; DH 2004). The birth plan should be discussed in full with the midwife looking after the woman in labour.
Hospital is an alienating environment for most women, in which institutionalised routines and lack of privacy can contribute to feelings of loss of control and disempowerment (Lock and Gibb 2003; Steele 1995).
The studies by Green et al. (1990) and Simkin (1992) found that control, or lack of it, was important to the women’s experience of labour and their subsequent emotional well-being.
Trials have demonstrated the benefits to women of having a low-risk, midwife-led area as an alternative to the conventional labour ward (Birthplace in England Collaborative Group 2011; Hodnett et al. 2010; Hatem et al. 2008; Byrne et al. 2000; Hodnett 2000; Waldenstrom 1997; Hundley et al. 1994; McVicar et al. 1993).
The non-labour ward or radically modified environment is associated with lower rates of analgesia, augmentation and operative delivery, as well as greater satisfaction with care and positive effect on care givers (Birthplace in England Collaborative Group 2011; Hodnett et al. 2010; Hodnett et al. 2009).
Midwives should be aware of the influence the physical environment has on their practice (Hodnett et al. 2010).
2 Evidence Based Guidelines for Midwifery-Led Care in Labour ©The Royal College of Midwives 2012
Birth Environment
The environment in which a woman labours can have a great effect on the amount of fear and anxiety she experiences.
Hospital is an alienating environment for most women, in which institutionalised routines and lack of privacy can contribute to feelings of loss
of control (Lock and Gibb 2003; Steele 1995).
Brown and Lumley (1994) found that the technology and intervention that has now become commonplace on many labour wards was implicated in women’s dissatisfaction with labour. Increased anxiety brought on through loss of control can interfere with the normal effective physiology of labour (Steele 1995).
The studies by Green et al. (1990) and Simkin (1992) found that control,
or lack of it, was important to the women’s experience of labour and their subsequent emotional wellbeing.
It is not easy to separate the influence of the model of care
from the physical environment on the outcomes.
Hodnett et al. (2010) discuss the effect that the physical environment can have on practice, within the supportive social model of care.
In 2009, Hodnett et al. undertook a pilot study aimed to investigate the impact of the physical environment on women and practitioners by making simple but radical modifications to a hospital labour room, which included the removal of the standard hospital bed and the addition of equipment to promote relaxation, mobility,
and calm.
The women were then randomly allocated either the modified or typical
labour room.
Though the pilot was small in numbers, the outcomes indicated that the physical environment modification had a positive effect on women and care providers.
The philosophy of mobilisation in active labour was increasingly supported in the modified environment (Hodnett et al. 2009).
RCM (2008) Birth Centre Standards for England Standard 7.6 sets criteria of
‘An environment that protects and promotes women’s privacy and dignity, respecting
their human rights and provides facilities to maintain adequate nutrition and hydration in labour.’
Respect for a woman’s wishes, and her involvement in decision-making is essential to her care in pregnancy and labour (DH 2007, DH 2004).
National Service framework maternity policy (DH 2004) pledged that service should “ensure that pregnant women receive high quality care throughout their pregnancy, have a normal childbirth wherever possible, are involved in decisions about what is best for them and their babies, and have choices about how and where they give birth” and the choice aspect remains within NHS future plans (DH 2010).
It would appear that women have better physical and emotional labour outcomes when they are involved in the decision making (Hodnett et al. 2010).
Green et al.’s study (1990) found that good information was important to a woman’s birth experience and also to her subsequent emotional well-being.
The decision-making must extend to the woman’s choice of companion(s), who should be made to feel welcome in the labour ward.
3
Evidence Based Guidelines for Midwifery-Led Care in Labour ©The Royal College of Midwives 2012
Birth Environment
Birth planning is a continuous part of antenatal care.
This requires a focussed discussion about place of birth, at which ‘women should receive clear, unbiased advice and be able to choose where they would like their baby to be born’ (DH 2007; DH 2004).
The recent Birthplace in England study (Birthplace in England Collaborative Group 2011) looked at safety of births planned in 4 different settings: home, freestanding midwifery units, alongside midwifery units and obstetric units for women with straightforward pregnancies.
It found that birth is safe wherever it takes place but there is a small but increased risk of adverse outcome for the neonate for nulliparous women associated with planned home birth.
The outcomes for multiparous or in other midwife led birth environments were the same. The study did not look into reasons for this and further exploration into the variation is required.
However, this information needs to be included in the discussions with women antenatally. The ‘birth talk’ and associated birth plan are essential opportunities for women and midwives to share information (NICE 2007).
The birth plan should be discussed in full with the midwife looking after the woman
in labour.
Women often find it difficult to ask questions, so midwives need to encourage them to do so, and to act as advocate for the wishes expressed (Kirkham 1986).
Trials have demonstrated the benefits to women of less intervention and more mobility, in having a low-risk, midwife-led area as an alternative to the conventional labour ward (Birthplace in England Collaborative Group 2011; Hodnett et al. 2010; Hatem et al. 2008; Byrne 2000; Hodnett 2000; Waldenstrom 1997; Hundley et al. 1994; McVicar et al.
1993). The philosophy behind the provision of such units is to provide a ‘homely’ environment, where women can take more control and labour is managed with minimal intervention (Hodnett et al. 2010; Hundley et al. 1994).
It has also been found that women who give birth in low-tech, midwife-led facilities, e.g. home or birth centres, require less pharmacological analgesia (Hodnett et al. 2010; Chamberlain et al. 1997; Skibsted and Lange 1992).
Hodnett et al.’s (2010) review found that the alternative birth setting environment is associated with lower rates of analgesia, augmentation and operative delivery, as well as greater satisfaction with care.
There was a non-statistically- significant trend towards higher perinatal mortality in the home-like setting, and the reviewers conclude that ‘an over-emphasis on normality’ may lead to delayed recognition of or action regarding complications.
Walsh (2004) has challenged this conclusion from his own experience and suggests that midwives who work in this environment are ‘astute assessors of normal birth’ and highly skilled practitioners, who are active in performing repeated emergency drills.
Hodnett et al. (2010) found, in their comparison of alternative and conventional labour and birth environments, that staff working in the ‘alternative’ settings all shared philosophies and guidelines that valued midwifery-led care.
The study was not able to explore the separate influences of the physical environment and models of care such as, for example, continuity of caregiver, but concluded that the impacts of midwifery-led care and the nature of the birth setting are fundamentally interdependent in the chain of cause and effect leading to more positive outcomes.
4
Evidence Based Guidelines for Midwifery-Led Care in Labour ©The Royal College of Midwives 2012
Birth Environment
References
Brown S, Lumley J (1994) Satisfaction with care in labour and birth: a survey of 790 Australian women. Birth 21(1): 4-13
Birthplace in England Collaborative Group (2011) Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: The Birthplace in England national prospective cohort study. British Medical Journal 343: d7400
Byrne J, Crowther C, Moss J (2000) A randomised controlled trial comparing birthing centre care with delivery suite care in Adelaide. Australia Australian and New Zealand Journal of Obstetrics and Gynaecology 40(3): 268-74
Chamberlain G, Wraight A, Crowley P (1997) Homebirths: The Report of the 1994 Confidential Enquiry by the National Birthday Trust Fund. Carnforth, Lancashire: The Parthenon Publishing Group
Department of Health (DH) (2010) Equity and Excellence: Liberating the NHS. London: HMS
Department of Health (2004) National Service Framework for Children, Young People and Maternity Services. London:DH
Green JM, Coupland VA, Kitzinger S (1990) Expectations, experiences and psychological outcomes of childbirth: a prospective study of 825 women. Birth 17(1): 15-24
Hatem M, Sandall J, Devane D et al. (2008) Midwife-led versus other models of care for childbearing women. Cochrane Database of Systematic Reviews, Issue 4. Chichester: John Wiley & Sons
Hodnett E, Downe S, Edwards N, et al. (2010) Alternative versus conventional institutional settings for birth. Cochrane Database of Systematic Reviews, Issue 9. Chichester: John Wiley & Sons
Hodnett ED, Stremler R, Weston JA, et al. (2009) Re-conceptualizing the hospital labor room: the Place (Pregnant and Laboring in an Ambient Clinical Environment) pilot trial. Birth 36(2):159-66
Hodnett ED, Hatem M, Sandall J, et al. (2008) Continuity of caregivers for care during pregnancy and childbirth. Cochrane Database of Systematic Reviews, Issue 4. Chichester: John Wiley & Sons
Hodnett ED (2000) Continuity of caregivers for care during pregnancy and childbirth. Cochrane Database of Systematic Reviews 2000, Issue 1. Chichester: John Wiley & Sons
Hundley V, Cruikshank F, Lang G, et al. (1994) Midwife managed delivery unit: a randomised controlled comparison with consultant led care. British Medical Journal 309(6966): 1400-1404
Kirkham MJ (1986) A feminist perspective in midwifery. In Webb C (ed.) Feminist practice in women’s health care. Chichester: John Wiley
Lock L, Gibb H. (2003) The Power of Place. Midwifery 19(2): 132-139
McVicar J, Dobbie G, Owen-Johnston L, Jagger C, et al. (1993) Simulated home delivery:
a randomised control trial. British Journal of Obstetrics and Gynaecology 100(4): 316-33
National Institute of Clinical Excellence (NICE) (2007) Intrapartum care: management and delivery of care to women in labour. London: NICE
The Royal College of Midwives (RCM) (2008) Standards for birth centres in England: a standards document. London: RCM
Simkin P (1992) Just another day in a woman’s life? Part 2 Nature and consistency of women’s long-term memories of their first birth experiences. Birth 19(2): 64-81
Leyla Mollamahmutoğlu,1 Özlem Moraloğlu,1 Şebnem Özyer,1 Filiz Akın Su,1 Rana Karayalçın,1 Necati Hançerlioğlu,1Özlem Uzunlar,1 and Uğur Dilmen2
Objective
To document the practice of labour in water, to assess the effects of water immersion during labor and/or birth (labour stages 1, 2 and 3) on maternal, fetal and neonatal wellbeing and to compare the outcomes and safety with conventional vaginal deliveries and deliveries with epidural analgesia.
Material and Methods
Two-hundred and seven women electing for waterbirth (n=207) were compared with women having conventional vaginal deliveries (n=204) and vaginal deliveries with epidural analgesia (n=191). Demographic data, length of 1st, 2nd and 3rd stage of labor, induction and episiotomy requirements, perineal trauma, apgar scores, NICU requirements and VAS scores were noted.
Results
The 1st stage of labor was shorter in waterbirths compared with vaginal delivery with epidural analgesia but the 2nd and 3rd stage of labor were shortest in patients having waterbirth compared with conventional vaginal delivery and vaginal delivery with epidural analgesia.
Patients having waterbirth had less requirement for induction and episiotomy but had more perineal laceration. All women having waterbirths had reduced analgesia requirements and had lower scores on VAS.
There was no difference in terms of NICU admission between the groups. Apgar scores were comparable in both groups. There were no neonatal deaths or neonatal infections during the study.
Conclusion
The study demonstrates the advantages of labor in water in terms of reduction in 2nd and 3rd stage of labor, reduction in pain and obstetric intervention such as induction or amniotomy.
Introduction
In 1983, Odent published the results of the first hundred water births in The Lancet (1). It was postulated that anxiety and pain may trigger a stress response during labour (2) leading to reduced uterine activity and dystocia (3). Labouring in water may overcome this stress response by aiding relaxation and relief of pain (4).
Zanetti-Daellenbach et al. revealed that water deliveries performed in a selected low risk collective needed less analgesia had a shorter duration of first and second stages of labour, a lower episiotomy rate and were not associated with any adverse maternal or fetal outcome (5).
The advantages of immersion in water during labour and/or birth include reduced pain, increased functional diameter of the true pelvis, increased quality of contractions, increased release of endorphins, decreased need for opiates, increased movement for the mother as well as improved positioning in different stages of labour (6).
There are also studies that have reported the disadvantages associated with water birth which include maternal and neonatal infections, as well as the possibility of respiratory problems for the newborn (7, 8).
Cluett and Burns in a review of 11 trials concluded that water immersion during the first stage of labour reduced the use of epidural/spinal analgesia, but there was limited data for other outcomes related to water use during the first and second stages of labour (9). They also stated that there was no evidence of increased adverse effects on the fetus/neonate or woman from labouring in water (9).
The aim of this study is to document the practice of labour in water, to assess the effects of water immersion during labour and/or birth (labour stages 1, 2 and 3) on maternal, fetal and neonatal wellbeing and to compare the outcomes and safety with conventional vaginal deliveries and deliveries with epidural analgesia.
Materials and Methods
In a prospective clinical trial, the interview and observation techniques were used to study 610 pregnant women who were admitted to Zekai Tahir Burak Women’s Health Education and Research Hospital, between June 2007 and September 2008.
Women electing for water birth (Study Group 1, n=207) were compared with vaginal deliveries with epidural analgesia (Study Group 2, n=191) and women having conventional vaginal deliveries (Control, n=204).
The pregnant women were given comprehensive information on water birth before they were asked to participate in the study. Ethical approval was obtained from the local research ethics committee prior to the study, and written informed consent obtained from all patients.
This study was conducted in accordance with the basic principles of the Helsinki Declaration.
The inclusion criteria were gestational age between 37–42 weeks, no previous history of cesarean section, intact membranes, absence of placental abruption or placenta previa, no malpresentation, normal sized single fetus, and normal results of fetal wellbeing tests. The pregnant women with medical or obstetric risk factors were excluded (n=8).
Women presenting on the delivery suite with painful uterine contractions had an initial cervical assessment. This was taken as the onset of the active phase of labour in all groups. They were assigned to control and two study groups. The women were put in a standardized warm water pool which is large enough to allow the pregnant women move freely.
At the time of delivery the water temperature was set to between 37 and 37.5ºC so that the baby was not stimulated to breathe underwater by the cooler temperature of the pool. Fetal heart monitoring was performed at regular intervals with Doppler or NST. In the second stage of labour, care was taken to ensure the controlled delivery of the head of the fetus.
The newborn was placed gently in the mother’s arms within seconds but without rushing and then the cord clamped and cut. Delivery of the placenta and the membranes was completed outside the pool. After the delivery, the pool was emptied and cleaned with antiseptic solution. Cultures were taken for the determination of pathogenic bacteria.
Demographic data, length of 1st, 2nd and 3rd stages of labor, requirement for induction and episiotomy, perineal trauma, apgar scores, neonatal intensive care unit (NICU) requirements and visual analog scale (VAS) scores were noted on a questionnaire.
The women evaluated their birth experience with the VAS (10 cm long VAS from 1 to 10 corresponding to the amount of pain felt by the woman with number 1 for no pain and with number 10 for dreadful pain).
Statistical analysis
Data were evaluated by SPSS for Windows release 15.0 (Chicago Inc.). To compare groups, we used the Chi-square test for categorical variables, Oneway ANOVA and Bonferroni tests for continuous variables that have normal distribution, Kruskall-Wallis oneway ANOVA for continuous variables that have no normal distribution.
As described, variables, frequencies and percentages were given for categorical variables, Mean±standard deviations and median were given for continuous variables. Alpha=0.05 was accepted as a statistically significant value.
In order to detect±2 percentage point difference in VAS scores between groups, for having alpha=0.05, power=0.97, it was predicted that approximately 200 subjects for each group should be taken (NCSS-Pass Pocket Program was used) (Chow SC et al.) (10).
The study groups consisted of 207 water births (Group 1) and 191 vaginal deliveries with epidural analgesia (Group 2), the control group (Group 3) of 204 patients gave birth by the conventional vaginal delivery method at the hospital. The women in the three groups were matched with respect to age, BMI and gestational age (Table 1).
There were 276 primigravidae and 326 multiparous women having water births (Table 2). The mean age of the women were 26.2±5.1, 26.1±4.5 and 25.5±5.1 respectively (Table 1). The mean cervical dilatation at admission in both group 1 (5.3 cm) and group 2 (4.6 cm) was not significantly different from group 3 (4.7 cm).
The duration of the 1st stage of labour was shortest in the conventional vaginal delivery group whereas the duration of the 2nd and the 3rd stages of labour were shortest in the water birth group (Table 1).
There was a highly significant reduction in the induction and episiotomy requirements in the water birth group (Table 1). VAS scores were the lowest in the water birth group, so there was less analgesia requirement (Table 1).
Conversely, the perineal laceration rate was higher in the water birth group, however most of these lacerations were minimal. Systolic and diastolic blood pressures seem to be lower in the water birth group, however the differences were not clinically significant. The decrease in hemoglobin levels as an indication of blood loss during labour were not statistically significant.
The birthweight of the infants were highest, however Apgar scores were slightly lower in the water birth group. There was no difference in the rates of admissions to the NICU between the groups (Table 1). There were no documented neonatal infections. There was no adverse perinatal outcome or neonatal deaths. All the babies were born in good condition.
When primigravidas and multiparous women having water birth are considered (Table 2), the 1st stage of labour is longer in both groups compared with controls, however the 2nd and 3rd stages of labour were the shortest in both primigravidas and multiparous women labouring in water compared with controls. The need for induction and episiotomy for both primigravidas and multiparous women was lowest in water birth group compared with others.
Perineal laceration rates were higher in both groups compared with controls. VAS scores were lowest in the water birth group in both primigravidas and multiparous women. Apgar scores were slightly lower in the water birth group, however NICU admission rates were not statistically different in the water birth group for both primigravidas and multigravidas.
Discussion
Water births have rapidly become one of the most popular birth methods. There is evidence of use of water immersion as a therapeutic medium for physical and psychological illnesses by the Chinese, Egyptians, Japanese and Assyrians, as well as Greeks and Romans (9).
Water immersion during labour, including birth, used for relaxation and pain relief, has a long history. In 1995, the first international water birth conference was held in London, followed by many researches and conferences.
The positive physiological effects of hydrotherapy can facilitate the neurohormonal interactions of labour, reducing pain, and potentially facilitates the progress of labour (11, 12). Water immersion may be associated with improved uterine perfusion, less painful contractions and a shorter labour with fewer interventions (13–15).
Several reports have shown that water immersion shortens the process of labour (1, 15), however some others found no significant difference for the duration of the 1st stages of labour (13, 16–20). The present study also demonstrates that the 1st stage of labour is not shortened by immersion in water in either primigravidas or multigravidas.
Cammu et al., Eckert et al., Rush et al. and Woodward et al. provided data on analgesia and anesthesia use in their studies and found that there was a significant reduction in the incidence of analgesia and anesthesia use among women placed in water during the first stage of labour (16, 17, 19, 20).
In the present study, we have shown that VAS scores indicating the pain felt by the women were lowest among women having water birth, even lower than the women labouring with epidural analgesia. In agreement with these studies, we observed that immersion in water greatly reduces the pain and need for additional analgesia.
Labouring in water has been found to reduce stress hormones and cathecolamines which inhibit oxytocin and labour progress (9). In our study, the duration of the second stage of labour was found to be shorter in water births, consistent with the results of studies of Chaichian et al. and Otigbah et al. (6, 21).
The fetus may be more likely to adopt a more relaxed and flexed position, because the mother can easily explore different positions to maximise her pelvic diameters (22).
The duration of the 3rd stage of labour, which is the delivery of the placenta, is also significantly reduced after water births. This minimizes amount of blood loss during this period.
The lower blood loss in water births can also be explained by the hydrostatic pressure in the pool, by the less severe lacerations or possibly by a facilitated control of the third stage of labour.
In the study, patients having waterbirth had less requirement for obstetric interventions such as induction and episiotomy but had more perineal lacerations. However, the lacerations in water birth group were less severe than those in epidural analgesia and conventional delivery group.
Otigbah et al. found that primigravidas having water births had less perineal trauma and the overall episiotomy rate was 5 times greater in the control group, but overall, more women having water births had perineal tears (21). On the other hand, there are studies which show no difference in perineal trauma (23, 24).
The reason why women having water births had more tears may be explained by the difficulty in accessing the women’s perineum during birth, resulting in more perineal trauma.
However, the widespread belief that with episiotomies 3rdand 4th degree lacerations are avoided is open to question, because in our study episiotomy rates were lowest after water births, and the lacerations were minimal.
There are some concerns about water birth for the fetus. These are thermoregulation during labour, infection and onset of respiration at birth. As the water temperature of the pool does not exceed the maternal body temperature, fetal hyperthermia and associated cardiovascular and metabolic disturbances will not occur (25). None of the newborns in our study took its first breath in water.
This has been explained by the diving reflex which shows that, when the face or especially the glottis comes in contact with fluid, respiration movements are inhibited. Aspiration will occur only when the diving reflex fails, because of anesthesia or severe asphyxia or because of the inappropriate pool temperature.
When we consider neonatal infection, several reported comparative studies, cohort studies and audits report no increased risk of infection to the newborn (5, 19, 21). This is also confirmed by the study that there were no documented neonatal infections.
Overall, water birth does not cause an increased risk of adverse effects to the fetus/newborn.
In conclusion, the study demonstrates the advantages of water birth in terms of reduction in the duration of the 2nd and 3rd stages of labor, reduction in pain and obstetric intervention such as induction or episiotomy.
Labouring in water significantly reduces pain and the requirement of epidural/spinal analgesia.
It is a management approach which contributes positively to maternal physiological and psychological health by reducing the augmentation which is known to increase the risk of uterine hyperstimulation and fetal hypoxia and by reducing the obstetric interventions which are associated with lower maternal satisfaction.
There is no increased adverse effects to the fetus or labouring women.
Water birth may be an alternative birth method that can be offered in selected patients.
Footnotes
Conflict of interest
No conflict of interest was declared by the authors.
References
1. Odent M. Birth under water. Lancet. 1983;2:1476–7. [PubMed]
2. Brownridge P. The nature and consequences of childbirth pain. Eur J Obstet Gynecol Reprod Biol. 1995;59:9–15. [PubMed]
3. De Punzio C, Neri E, Metelli P, Bianchi MS, Venticinque M, Ferdeghini M, et al. The relationship between maternal relaxation and plasma beta-endorphin levels during parturition. J Psychosom Obstet Gynaecol. 1994;15:205–10. [PubMed]
4. Elizabeth R, Cluett Ruth M, Pickering Kathryn, Getliffe Nigel, James St. George Saunders. Randomised controlled trial of labouring in water compared with standard of augmentation for management of dystocia in first stage of labour. BMJ. 2004;328:314–8. [PMC free article] [PubMed]
5. Zanetti-Daellenbach RA, Tschudin S, Zhong XZ, Holzgreve W, Lapaire O, Hösli I. Maternal and neonatal infection and obstetrical outcome in water birth. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2007;134:37–43. [PubMed]
6. Chaichian S, Akhlaghi A, Rousta F, Safavi M. Experience of water birth delivery in Iran. Arch Iran Med. 2009;12:468–71. [PubMed]
7. Rawal J, Shah A, Stirk F, Mehtar S. Water birth and infection in babies. BMJ. 1994;20:309, 511.[PMC free article] [PubMed]
8. Geissbühler V, Eberhard J. Experience with water births: a prospective longitudinal study of 9 years with almost 4,000 water births. Gynakol Geburtshilfliche Rundsch. 2003;43:12–8. [PubMed]
9. Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Database of Systematic Reviews. 2009;2:CD000111. [PMC free article] [PubMed]
10. Chow SC, Shao J, Wang H. Sample Size Calculation in Clinical Research. Second Edition. Chapman & Hall; New York: 2008. pp. 70–4.
11. Ginesi L, Niescierowicz R. Neuroendocrinology and birth 1: stress. British Journal of Midwifery. 1998;6:659–63.
12. Ginesi L, Niescierowicz R. Neuroendocrinology and birth 2: The role of oxytocin. British Journal of Midwifery. 1998;6:791–6.
13. Schorn MN, McAllister JL, Blanco JD. Water immersion and the effect on labor. J Nurse Midwifery. 1993;38:336–42. [PubMed]
14. Geissbuehler V, Eberhard J. Waterbirths a comparative study. Aprospective study on more than 2,000 waterbirths. Fetal Diagnosis and Therapy. 2000;15:291–300. [PubMed]
15. Burke E, Kilfoyle A. A comparative study, waterbirth and bed birth. Midwives. 1995;108:3–7.
16. Cammu H, Clasen K, Wettere L, Derde M-P. To bathe or not to bathe during the first stage of labor. Acta Obstet Gynecol Scand. 1994;73:468–72. [PubMed]
17. Eckert K, Turnbull D, MacLennan A. Immersion in water in the first stage of labour: a randomised controlled trial. Birth. 2001;28:84–93. [PubMed]
18. Kuusela P, Koivisto A-M, Heinonen PK. Lammin kylpy synnytyksen avautumisvaiheessa. [Warn tub bath during opening phase of labor]. Suomen Laakarilehti. 1998;11:1217–21.
19. Rush J, Burlock S, Lambert K, Loasley-Milman M, Hutchinson B, Enkin M. The effects of whirlpool baths in labour: a randomised controlled trial. Birth. 1996;23:136–43. [PubMed]
20. Woodward J, Kelly SM. A pilot study for a randomised controlled trial of waterbirth versus land birth. BJOG. 2004;111:537–45. [PubMed]
21. Otigbah CM, Dhanjal MK, Harmsworth G, Chard T. A retrospective comparison of water births and conventional vaginal deliveries. Eur J Obstet Gynecol Reprod Biol. 2000;91:15–20. [PubMed]
22. Ohlsson G, Buchhave P, Leandersson U, Nordstrom L, Rydhstrom H, Sjolin I. Warm tub bathing during labor; maternal and neonatal effects. Acta Obstet Gynecol Scand. 2001;80:311–4. [PubMed]
23. Lenstrup C, Schantz A, Berget A, Feder E, Rosen⊘ H, Hertel J. Warm tub bath during delivery. Acta Obstet Gynecol Scand. 1987;66:709–12. [PubMed]
24. Church LK. Water birth: one birthing center’s observations. Journal of Nurse-Midwifery. 1989;34:165–70. [PubMed]
25. Johnson P. Birth under water – to breathe or not to breathe. BJOG. 1996;103:202–8. [PubMed]

Megan Cooper RM, BHSc (Honours), Jane Warland RM, PhD Helen McCutcheon RM, PhD.
Abstract
Water immersion for labour and birth is becoming an increasingly attractive option for women.
However, with what has been described as a paucity of research, water immersion policies appear to lack the evidence to ensure confidence in their use, safety in their implementation and importantly, acknowledgement of women’s autonomy to utilise water for labour and birth irrespective of their perceived ‘risk’.
In touching on the difficulties experienced by maternity care providers working within a system largely dominated by a ‘risk adverse’ paradigm, the following paper will highlight the shortfalls of research surrounding water immersion for labour and birth and the difficulties of utilising policies informed almost entirely by this research.
The current paucity of rigorous evidence and the difficulties faced by maternity care providers facilitating the option, highlights that greater emphasis needs to be placed on gaining a substantial evidence-base to inform future water immersion polices with more weight given to both observational data and anecdotal experience.
Future research should focus on both quantitative and qualitative aspects of water use for labour and birth to ensure that policies incorporate the required risk/benefit analysis, the opportunity for shared and informed decision-making and ultimately, the facilitation of woman-centred care.
Should we throw out the bath water?
For many women water immersion (WI) during labour and birth is an attractive and sought after option of care.
Despite the availability of literature surrounding WI for labour and birth many argue that high quality research with which to measure risks and benefits is still lacking.
As the option has become increasingly available, the development of policy to guide and inform care providers in the safe practice of WI for labour and birth has become necessary.
Consequently, policies appear to have been derived from what some describe as a less than substantive evidence-base (Cluett and Burns, 2009).
This has elicited debate as to whether the practice itself and therefore the policies currently informing the practice reflect the required foundational evidence to fulfill the ideal of evidence-based practice.
In touching on the current difficulties experienced by care providers working within in a ‘risk averse’ system the following paper will briefly explore WI for labour and birth, highlight the perceived shortfalls of research pertaining to its practice and discuss some of the difficulties of undertaking research at the level that many believe is required.
The role of qualitative research in informing the practice of labour and birth in water will also be examined with particular reference to the goal of woman-centred care and the need for policy that is reflective of a holistic evidence-base and supportive of women’s experience, satisfaction and choice.
The practice of water immersion for labour and birth
Despite common belief, WI for labour and birth is not a new phenomenon, with history dating back to the Egyptian Pharaohs and the Minoans of Crete (Mackey, 2001). In the 1960’s, Igor Charkovsky, a Russian midwife, began experimenting with the use of water for labour and birth after realising the positive physical and physiological effects of WI (Houston, 2010).
The 1980s saw Michel Odent, a well-known French Obstetrician and arguably the pioneer of modern water birth, establish the first birthing unit allowing women access to baths during labour, many of whom also went on to birth in water
(Houston, 2010). His observations and documented accounts of witnessing women immerse themselves in warm water allowed him to become a major influential figure in the global water birth movement and in the education of practitioners who facilitate the option of WI.
The advantages and benefits of WI during labour and birth have for the most part, not been thoroughly investigated through rigorous research.
Documented benefits include reductions in pharmacological pain relief (Eberhard et al., 2005, Otigbah et al., 2000, Benfield et al., 2001, Cluett and Burns, 2009), reduced blood loss and perineal trauma (Cluett and Burns, 2009) as well as facilitation of dysfunctional labour (Benfield et al., 2010, Cluett et al., 2004).
It has long been held that water immersion facilitates ‘normal’ birth and the latest prospective and descriptive cross sectional research findings provide support for this belief (Burns et al., 2012, Dahlen et al., 2012).
Burns et al. (2012) found that there was a higher frequency of spontaneous birth in nulliparas and greater rates of normal birth in both nulliparous and multiparous women when water was used during labour and/or birth. More specifically, of the 8924 participants almost 90 percent had a spontaneous birth and of these 5192 (58.3%) of women birthed in water.
Further support for benefits of water use come from Dahlen et al. (2012). They found in their Australian descriptive cross sectional study that women birthing in water had lower rates of major perineal trauma and PPH ≥ 500 milliliters when compared with those who used a birth stool on land.
Improved APGAR scores at five minutes were also noted for babies born into water compared to those whose mothers birthed in a semi-recumbent position on land although the authors note that they are unsure as to whether a semi- recumbent position was favoured by practitioners when there were fetal concerns, thereby potentially impacting on the results.
However, what is perhaps most important in terms of these findings is that there were no documented increased adverse outcomes for mothers who utiliszed water during labour and birth nor were there statistically significant increases in unfavourable outcomes for babies born into water.
Anecdotal experience supports these benefits further, with women suggesting greater levels of satisfaction, sense of autonomy and care providers observing less use of pharmacological pain relief and the facilitation of the fourth stage of labour, particularly in the initiation of breastfeeding.
Qualitative researchers have also found that women who birth in water feel protected, safe, relaxed and in control (Benfield et al., 2010, Maude and Foureur, 2007, Benfield, 2002).
For example, one New Zealand interpretive study, conducted by Maude and Foureur (2007), highlighted that WI provided a ‘sanctuary’ or environment whereby women felt protected and sheltered from intervention and interference. Participants also voiced a reduction in the fear of the birthing process and pain.
For many maternity care providers, water use for labour and birth is viewed as a method of providing women an alternative method of pain relief, ease of position changes and relaxation (Gilbert and Tookey, 1999, Meyer et al., 2010, Maude and Foureur, 2007, Woodward and Kelly, 2004, Stark and Miller, 2009).
Although evident throughout the literature, the observation and experience of maternity care providers is often challenged against minimal scientific proof, which to date, is still not entirely definitive.
Conversely, many continue to challenge the use of water for labour and birth claiming that it is neither normal nor natural for land living mammals to birth into water and that there exist too many associated ‘risks’ and adverse outcomes to mother and infant (Kassim et al., 2005, Mammas and Thiagarajan, 2009, Carpenter and Weston, 2011, Pinette et al., 2004).
The most recent published adverse outcomes pertaining to the use of water immersion during labour and birth come from Soileau et al. (2013) and Menakaya et al. (2012). Soileau et al. (2013) documents a neonatal infection and subsequent neonatal demise post a home water birth attributed to a maternal diarrheal infection in the week prior to birth. The infection believed to have been transmitted to the neonate after the mother defecated in the bath during labour.
This provides justification and support for the use of policy and/or guidelines in guiding practitioners in the facilitation of the option. Furthermore, its draws attention to the knowledge and understanding practitioners must attain in order to make decisions that ensure both maternal and neonatal wellbeing and safety when water is used.
Although Menakaya et al. (2012) did not assess maternal or neonatal infections in their retrospective design of 216 Australian women birthing in water, they noted that babies born into water showed a statistically significant difference in APGAR scores less than or equal to seven at one minute and as well as admission to Special Care Nursery (SCN) post birth in the water birth group.
Interestingly, three of the neonates transferred to SCN were admitted for feeding difficulties, issues which cannot be definitely linked to water immersion, one was admitted post a mild shoulder dystocia which presumably required the woman to be evacuated from the bath prior to birth and one for meconium aspiration, suggesting the presence of meconium which is commonly cited contraindication to birthing in water.
The remaining infants were admitted for resuscitation and an apneic event, which are also not unique to infants born in water.
One infant in the control group was admitted to the SCN and was transferred for respiratory distress requiring the longest stay of all infants admitted to the SCN. These findings are dissimilar to those of Mollamahmutoglu et al. (2012) who found no instance of neonatal infection and no significant difference in admission to the Neonatal Intensive Care Unit (NICU) when comparing infants who were born in water with those who were not. These findings are indicative of the inconsistent and contradictory findings pertaining to the use of water for labour and birth across the literature.
As a result, empirical research has failed to provide a definitive risk/benefit analysis relating to WI for labour and birth particularly in terms of maternal and neonatal infection, neonatal SCN/NICU admission, perineal trauma and the incidence of neonatal drowning and water embolism, as examples.
Furthermore, the ongoing reference to ‘potential’, ‘possible’ and ‘theoretical’ risks throughout the literature as well as throughout policy and guideline documents creates difficulty and uncertainty as to what actually constitutes risk and what is deemed as safe when WI is utilised for labour and/or birth (Kvach and Martonffy, 2012, Mackey, 2001, Pinette et al., 2004).
Watering down practice
Maternity care providers aim as far as possible, to deliver care which is women- centered (Carolan and Hodnett, 2007). Woman-centered care (WCC) incorporates the requirement of a woman making informed choices about all aspects of her care through the sharing of information (Leap, 2009).
Maternity care providers hold information that is vital to the woman but given the need to work within protocols and guidelines, may at times provide information to meet institutional and personal expectations and commitments resulting in what Carolan and Hodnett (2007) describe as “rule following and avoidance of responsibility”.
Although not necessarily a deliberate attempt to limit the information and options available to women, difficulties can arise as maternity care providers walk the fine line between meeting obligations as the woman’s advocate and the demands of institutional policies, guidelines and regulations.
Consequently care providers may forsake their role as the woman’s advocate, and instead support an environment that fosters informed compliance (Carolan and Hodnett, 2007).
Unfortunately the ideal of woman-centredness is often relinquished particularly as birth has become viewed a process that requires management and medical influence (Kitzinger, 2006, Davis-Floyd, 2001).
The burden of ‘proof’ and necessity of evidence to support or refute ‘alternative’ options irrespective of women’s requests and subjective knowingness that they work (Klein et al., 2006) has been significant in the debate surrounding water immersion for labour and birth.
Many of the benefits that water provides the labouring and birthing woman are also what may deter care providers from offering it as an option. Women and care providers alike, have suggested that water provides safety, sanctuary and distance from the rest of world allowing women a sense of control and ownership over their labour and birth (Maude and Foureur, 2007). However, this protection from intervention and intrusion
ultimately means that the contemporary methods of monitoring and gauging progress are no longer as accessible or practical. For many practitioners the inability to monitor and assess women as they normally would results in fear, not only of litigation and ‘what if’s’ (Garland, 1919), but also of the practice itself.
Combatting fear and anxiety could be as easy as encouraging care providers to witness women using water during labour and birth, but opinion and bias in disfavour of water immersion demands the current ‘gap’ in research be bridged.
Furthermore, ethical practice calls for practitioners to dissociate personal bias and views from their practice to ensure women’s autonomy and ability to exercise choice are not downplayed or absent in the facilitation of care (ANMC, 2008, ANMC et al., 2008).
This issue is further complicated by the political climate within which maternity care now exists. Despite many care providers supporting the implementation and practice of WI for labour and birth and having the capacity and accreditation to facilitate the practice, they may be restricted by the lack of institutional resources and support (Garland, 2011) and most commonly, policy that is derived from an aversion of risk and research that has yet to determine with any certainty the safety of using water for labour and birth.
WI for labour and birth, despite putting what feels like an ‘alternative’ slant on care, has the potential as a practice and option of care, to assist care providers such as midwives to re-recognize normal physiological birth and subsequently work towards fulfilling the ultimate goal of woman-centred care.
A drought of evidence?
Water birth, in particular, is frequently associated with perceived risks and dangers and for this reason its use continues to be challenged relative to safety implications for mother and infant as has previously been discussed (Pinette et al., 2004, Kvach and Martonffy, 2012).
The conundrum is yet to be resolved particularly given the perceived paucity of definitive evidence. Yet the option is becoming increasingly demanded and therefore available and as a result, policies are in place to guide care providers in its facilitation, which are probably based (at least in part) on this limited evidence.
Although a number of attempts have been made to undertake research at the ‘gold’ standard, randomised controlled trials (RCTs) examining WI for labour and birth have suffered from less than optimal sample sizes, selection bias or poorly controlled confounding factors in groups of low risk women who are usually highly passionate and motivated (Woodward and Kelly, 2004, Schroeter, 2004, Cluett and Burns, 2009).
This is evident in the latest Cochrane review that included only 12 suitable studies, and of these, only three examined the use of water during second stage of labour (Cluett and Burns, 2009). Further to this there is currently no population level data being collected anywhere in the world about outcomes of WI nor even how many women choose to use WI in labour and/or birth in water (Pinette et al., 2004).
Undertaking the recommended research on WI and birth particularly such as the RCT suggested by Davies (2010) is complicated given that randomising for such a study brings about ethical and moral concerns.
Hendrix et al. (2009) found this to be the case in their Dutch questionnaire-based study assessing women’s reasons for not participating in an RCT investigating home birth versus hospital birth. Eighty-four women indicated that they did not participate due to a concern that they would be randomised to the ‘wrong’ group.
Woodward and Kelly (2004) attempted to overcome women’s reluctance to participate in their pilot RCT comparing water birth with land birth by including a ‘preference arm’. Their results indicated there were no significant difference noted between women who were randomised and those who chose the ‘preference arm’ and therefore concluded that women would be happy to be randomised in future and similar trials.
However, criticism of this RCT highlights that their sample size was too small and therefore underpowered to determine safety, particularly given that only 10 women birthed in water. Further to this, Keirse (2005) challenges the validity and generalisability given the ‘preference arm’ and the bias that meant only 20 of the 60 women who had a strong preference for one of the two options, were allocated to their preferred option.
Subsequently, randomisation of women to options of care, which elicit both emotive and somewhat passionate views, such as the use of WI in labour and birth, is not ethically or practically feasible particularly where recruitment of large numbers would be required to determine with any certainty the morbidity and mortality of the intervention.
The proposed undertaking of this type of randomised research is further complicated by inconsistency across institutional policies in addition to funding, necessary infrastructure and available accredited staff (Garland, 2011).
Not only does this make it difficult to allow for the option and implementation of WI for labour and birth but it also inadvertently contributes to the lack of evidence in that accessibility is limited and therefore data on resulting outcomes, scarce. Furthermore, where it is consistently highlighted that high quality evidence is deficient, the question must be asked: who or what is informing the policies already in existence?
Initiating a wave of change
It is consistently highlighted that there is insufficient data to inform the practice of labour and birth in water, but is this really the case? It is clear that there is a paucity of evidence in terms of empirical investigation however volumes of anecdotal experience and observational data are available suggesting that water has significant and undeniable benefits to the women, and arguably to the baby.
Despite its availability, little weight is given to this valuable information, information that could be informing the movement forward and providing direction for future investigation of WI for labour and birth.
There is no denying that greater high level research would be advantageous to providing a definitive set of benefits and risks and therefore, greater insight into the relative safety of WI for labour and birth. However, is a RCT the right option?
The suggestion that rigorous evidence is needed to inform policies and guidelines with confidence and reliability could be attributed to what has been termed the ‘medicalisation’ of pregnancy and birth (Brubaker and Dillaway, 2009, Benoit et al., 2010) particularly where the measure of risk is at the forefront of maternity care facilitation.
However, in a risk-averse climate, adverse events whether recognised through well-constructed studies, auditing or anecdotal accounts, are generally the first to be documented so as to prompt review of practice.
Despite this, a search of the literature surrounding WI for labour and birth highlights very few documented adverse outcomes at any level of evidence and of those that are documented; the outcomes cannot always be definitively attributed to the use of water (Pinette et al., 2004, Cluett and Burns, 2009, Byard and Zuccollo, 2010).
What are readily available are anecdotal and observational accounts that suggest that WI has extensive benefits, not only to the woman but also to birth outcomes. It could therefore be argued that quantitative research alone is insufficient to provide answers to myriad of complexities, questions and queries relating to the practice of WI for labour and birth and therefore, insufficient when informing policies particularly where women choose to exercise self-determination and choice irrespective of their perceived risk.
Freeman and Griew (2007) touch on this in their review of one WI policy and its development. Their findings suggest that policy could further be enhanced by placing weight on the views and experiences of consumers and addressing the importance of informed and shared decision making.
This calls for attitudinal change not only to facilitate care that is woman-centred but also to ensure that women’s autonomy is factored into the development and implementation of policies underpinning practice.
The significance and value of qualitative evidence is slowly being realised, particularly in maternity care where WCC is the ideal. Despite this, empirical evidence is still commonly viewed as more rigorous and therefore more reliable.
This is none too clear in the hierarchies of evidence that fail to give weight to qualitative investigation (Spiby and Munro, 2009). However, as health care moves towards patient-centred models, or woman-centredness (Leap, 2009), as is the case in maternity care, there is the need for increasing weight to be also placed on experience and opinion particularly surrounding policy formation and care facilitation.
In light of this, a multi-faceted evidence-based approach to policy development and implementation of WI for labour and birth is likely to be advantageous.
However, before recommendations can be made, a critical analysis of existing policies and their development should occur in order to highlight whether the so-called scarcity of evidence poses difficulties for those involved in WI policy formation and to what extent policy facilitates and/or restricts water use practice and more importantly, women’s autonomy.
Pooling for the future
This paper has touched on the many shortfalls of WI research to date as well as foreseeable difficulties of future research surrounding WI for labour and birth. Future research requires greater emphasis on both the quantitative and qualitative aspects of water use for labour and birth to ensure that policies incorporate both the risk/benefit analysis as well as the opportunity for shared and informed decision-making.
This includes greater exploration of the experiences and perceptions of women and importantly, an examination of current WI policies to determine how they are informed and developed and to what extent they facilitate the practice and support women’s autonomy.
Not only is there the potential for this all-encompassing research to assist maternity care providers in working with autonomy as practitioners and ensuring their ability to advocate for women but there is also the potential for the use of water for labour and birth to have positive outcomes in a system that has an ever increasing rate of intervention and deviation from what can be both a normal and natural process.
References
ANMC 2008. Code of Professional Conduct for Midwives in Australia, Dickson, ANMC.
ANMC, ACM & ANF 2008. Code of Ethics for Midwives in Australia, Dickson, ANMC.
BENFIELD, R. 2002. Hydrotherapy in labor. J Nurs Scholarsh, 34, 347-52.
BENFIELD, R., HERMAN, J., KATZ, V. L., WILSON, S. P. & DAVIS, J. M. 2001. Hydrotherapy in labor. Research in Nursing & Health, 24, 57-67.
BENFIELD, R., HORTOBÁGYI, T., TANNER, C., SWANSON, M., HEITKEMPER, M. & NEWTON, E. 2010. The Effects of Hydrotherapy on Anxiety, Pain, Neuroendocrine Responses, and Contraction Dynamics During Labor. Biological Research for Nursing, 12, 28-36.
BENOIT, C., ZADOROZNYJ, M., HALLGRIMSDOTTIR, H., TRELOAR, A. & TAYLOR, K. 2010. Medical dominance and neoliberalisation in maternal care provision: The evidence from Canada and Australia. Social science & medicine, 71, 475-481.
BRUBAKER, S. J. & DILLAWAY, H. E. 2009. Medicalization, natural childbirth and birthing experiences.Sociology Compass, 3, 31-48.
BURNS, E. E., BOULTON, M. G., CLUETT, E., CORNELIUS, V. R. & SMITH, L. A. 2012. Characteristics,Interventions, and Outcomes of Women Who Used a Birthing Pool: A Prospective Observational Study. Birth.
BYARD, R. W. & ZUCCOLLO, J. M. 2010. Forensic issues in cases of water birth fatalities. Am J Forensic Med Pathol, 31, 258-60.
CAROLAN, M. & HODNETT, E. 2007. ‘With woman’ philosophy: examining the evidence, answering the questions. Nursing Inquiry, 14, 140-52.
CARPENTER, L. & WESTON, P. 2011. Neonatal respiratory consequences from water birth. J Paediatr Child Health.
CLUETT, E. & BURNS, E. 2009. Immersion in water in labour and birth. Cochrane Database Syst Rev, CD000111.
CLUETT, E., PICKERING, R., GETLIFFE, K. & SAUNDERS, N. 2004. Randomised controlled trial of labouring in water compared with standard of augmentation for management of dystocia in first stage of labour. BMJ, 328, 314.
DAHLEN, H. G., DOWLING, H., TRACY, M., SCHMIED, V. & TRACY, S. 2012. Maternal and perinatal outcomes amongst low risk women giving birth in water compared to six birth positions on land. A descriptive cross sectional study in a birth centre over 12 years. Midwifery.
DAVIES, M. 2010. Water births and the research required to assess the benefits versus the harms. Journal of Paediatrics and Child Health.
DAVIS-FLOYD, R. 2001. The technocratic, humanistic, and holistic paradigms of childbirth. International Journal of Gynecology & Obstetrics, 75, S5-S23.
EBERHARD, J., STEIN, S. & GEISSBUEHLER, V. 2005. Experience of pain and analgesia with water and land births. Journal of Psychosomatic Obstetrics and Gynecology, 26, 127-133.
FREEMAN, L. M. & GRIEW, K. 2007. Enhancing the midwife-woman relationship through shared decision making and clinical guidelines. Women Birth, 20, 11-5.
GARLAND, D. 1919. Waterbirth: An attitude to care, Books for Midwives Pr.
GARLAND, D. 2011. Water birth: a way of enhancing and promoting normality. Promoting Normal Birth:Research, Reflections and Guidelines. 1st ed.: Fresh Heart Publishing.
GILBERT, R. E. & TOOKEY, P. A. 1999. Perinatal mortality and morbidity among babies delivered in water:surveillance study and postal survey. BMJ, 319, 483-7.
HENDRIX, M., VAN HORCK, M., MORETA, D., NIEMAN, F., NIEUWENHUIJZE, M., SEVERENS, J. & NIJHUIS, J. 2009. Why women do not accept randomisation for place of birth: feasibility of a RCT in The Netherlands. BJOG, 116, 537-42; discussion 542-4.
HOUSTON, J. 2010. Exploring the theories around use of water for labour and for birth. MIDIRS Midwifery Digest, 20, 343-347.
KASSIM, Z., SELLARS, M. & GREENOUGH, A. 2005. Underwater birth and neonatal respiratory distress. BMJ, 330, 1071-2.
KEIRSE, M. J. 2005. Challenging water birth — how wet can it get? Birth, 32, 318-22.
KITZINGER, S. 2006. Birth crisis, Routledge.
KLEIN, M. C., SAKALA, C., SIMKIN, P., DAVIS‐FLOYD, R., ROOKS, J. P. & PINCUS, J. 2006. Why do women go along with this stuff? Birth, 33, 245-250.
KVACH, E. & MARTONFFY, A. I. 2012. Are there any risks to a water birth?
LEAP, N. 2009. Woman-centred or women-centred care: does it matter? British Journal of Midwifery, 17, 12-16.
MACKEY, M. M. 2001. Use of water in labor and birth. Clin Obstet Gynecol, 44, 733-49.
MAMMAS, I. N. & THIAGARAJAN, P. 2009. Water aspiration syndrome at birth – report of two cases. J Matern Fetal Neonatal Med, 22, 365-7.
MAUDE, R. M. & FOUREUR, M. J. 2007. It’s beyond water: Stories of women’s experience of using water for labour and birth. Women and Birth, 20, 17-24.
MENAKAYA, U., ALBAYATI, S., VELLA, E., FENWICK, J. & ANGSTETRA, D. 2012. A retrospective comparison of water birth and conventional vaginal birth among women deemed to be low risk in a secondary level hospital in Australia. Women Birth.
MEYER, S. L., WEIBLE, C. M. & WOEBER, K. 2010. Perceptions and practice of waterbirth: a survey of Georgia midwives. J Midwifery Womens Health, 55, 55-9.
MOLLAMAHMUTOĞLU, L., MORALOĞLU, Ö., ÖZYER, Ş., SU, F. A., KARAYALÇıN, R., HANÇERLIOĞLU, N.,
UZUNLAR, Ö. & DILMEN, U. 2012. The effects of immersion in water on labor, birth and newborn and comparison with epidural analgesia and conventional vaginal delivery. Journal of The Turkish German Gynecological Association, 13, 45-9.
OTIGBAH, C. M., DHANJAL, M. K., HARMSWORTH, G. & CHARD, T. 2000. A retrospective comparison of water births and conventional vaginal deliveries. Eur J Obstet Gynecol Reprod Biol, 91, 15-20.
PINETTE, M. G., WAX, J. & WILSON, E. 2004. The risks of underwater birth. Am J Obstet Gynecol, 190, 1211-5.
SCHROETER, K. 2004. Water births: a naked emperor. Pediatrics, 114, 855-8.
SOILEAU, S. L., SCHNEIDER, E., ERDMAN, D. D., LU, X., RYAN, W. D. & MCADAMS, R. M. 2013. Case report: Severe disseminated adenovirus infection in a neonate following water birth delivery. J Med Virol, 85, 667-9.
SPIBY, H. & MUNRO, J. 2009. The development and peer review of evidence-based guidelines to support midwifery led care in labour. Midwifery, 25, 163-71.
STARK, M. A. & MILLER, M. G. 2009. Barriers to the use of hydrotherapy in labor. JOGNN: Journal of Obstetric, Gynecologic & Neonatal Nursing, 38, 667-675.
WOODWARD, J. & KELLY, S. M. 2004. A pilot study for a randomised controlled trial of water birth versus land birth. BJOG: An International Journal of Obstetrics and Gynaecology, 111, 537-545.
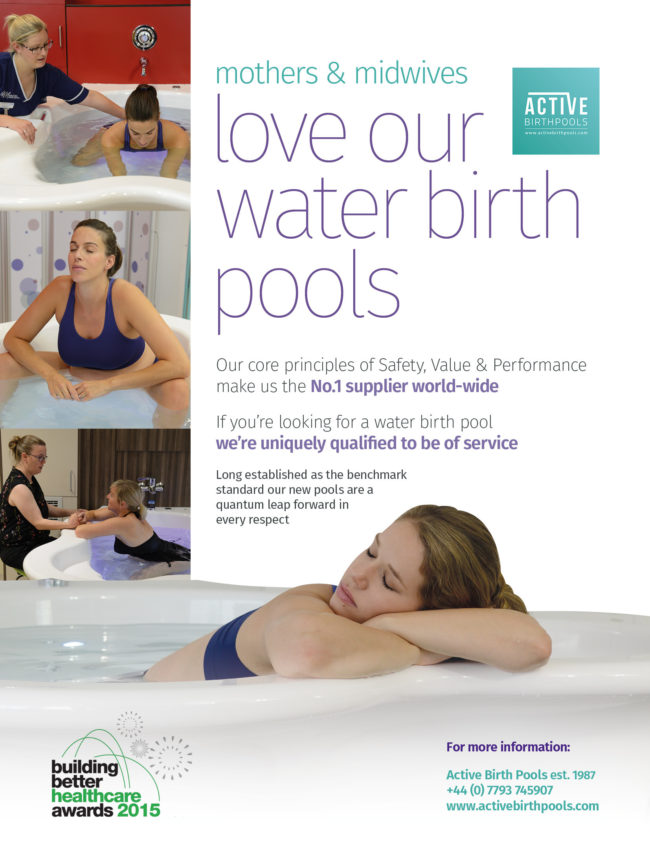
In light of the publication of recent articles that report the growing demand from women around the world who want to have a natural, drug free, non-medicalised birth (Weiss 2014 and Gilbert 2015) we need to look at ways to help them have this experience.
If they are not going be reliant on analgesia for pain relief they need options to help them cope with the pain to allow a physiological labor to unfold.
Immersion in warm water has been unequivocally proven to be of great benefit both physiologically and psychologically.
It is not important if the baby is born in water.
In fact, water birth should be de-emphasised as it is a controversial issue in many parts of the world.
The key point and main benefit that needs to be made and focused on is how women who enter a warm pool of water in established labour with strong contractions find that they are able to cope with the pain and have a natural birth.
Women have a greater sense of fulfillment and accomplishment and babies experience a non-traumatic birth.
Aside from the obvious benefits to mothers and babies, midwives experience greater job satisfaction and hospitals save money and optimise resources from the reduced use of analgesia, medical intervention and shorter hospital stays.
Nearly a third of women benefited from the use of a water birth pool in the UK in 2014 (National Maternity Survey 2014).
With up to 60% of mothers open to natural birth now is the time for midwives, obstetricians and hospitals to consider making this safe, low cost option available.
Studies have shown that upright labour positions are associated with a reduced second stage, fewer episiotomies or instrumental intervention in contrast to mothers labouring on their backs. (Gupta, Hofmeyr and Shehmar 2012 and Gupta and Nikodem 2000).
Many women also feel empowered in an upright position, and experience a sense of control over their labour (Balaskas 2001).
On land women need to contend with the force of gravity that limits their ability to assume upright postures especially as labour progresses and they feel tired.
Many women do not have the fitness or stamina to maintain upright postures for lengths of time. (Gupta JK, Hofmeyr GJ, Smyth R 2007).
The transition from the land to water helps revive and energise the mother giving her a new lease on life and sense of purpose.
The buoyancy of water supports the mother reducing her relative weight by approx. 33% (Archimedes Principle) allowing her to easily explore the full range of beneficial upright positions in comfort and move in ways that were not possible on land.
The calming, relaxing effect of the warm water promotes the flow of oxytocin, a powerful hormone that plays a huge role in childbirth, causing the uterus to contract and triggering the ‘fetal ejection reflex’.
Michel Odent has expounded upon the beneficial physiological effect that immersion in water during labour has on hormone secretion, including observations that women entering warm water experience oxytocin surges which can advance dilation and stimulate contractions (Odent 2014).
The space, depth and design features of Active Birth Pools allow women to move freely to find and be supported in the upright positions that are most comfortable and beneficial for a physiological labor to unfold.
There is evidence that water emersion in labour offers women a safe and effective form of pain relief in labour to those women who meet the criteria (NICE, 2007; NICE, 2014; Garland, 2011).
The use of telemetry provides women greater choice and control over their birth experience to facilitate the use of water (Birthing Pool or Bath) in labour and birth where their pregnancy and labour has been categorised as high risk and requires continuous fetal monitoring.
The Standard Operating Procedure (SOP) has been written to facilitate continuous fetal monitoring of high risk women in labour and birth who wish to use the birthing pool / water.
Telemetry is a wireless fetal monitoring device which facilitates continuous toco graph (CTG) monitoring where clinically indicated in the first and second stage of labour on a consultant led delivery suite.
Prior to the woman being offered the use of the birthing pool on the Delivery Suite consideration should be given to the plan of care and requirements of the woman and baby having reviewed the fully ante natal history.
The following lists are not exhaustive and full clinical assessment should be made on admission to delivery suite.
Click here for a copy of these guidelines

In recent years, professional organizations that represent maternal-child health care providers have taken various positions on the recommended use of immersion hydrotherapy during labor and birth. The resulting lack of consensus has made consistent and equitable access to this non-pharmacologic method for pain relief in labor challenging.
This model practice template was jointly developed by representatives from the American Association of Birth Centers, American College of Nurse-Midwives, Midwives Alliance of North America, National Association of Certified Professional Midwives, and other experts to offer guidance to health care professionals and institutions that provide or are implementing hydrotherapy services. This document is informed by the most current available information and resources that support best practices and serves as an outline of the various roles and responsibilities involved in providing hydrotherapy during labor and birth. Limited information has been published on the efficacy and safety of specific care practices before, during, or after hydrotherapy. However, this document is informed by the methodologically-sound, peer-reviewed studies that have been published to date. The format of this model practice template allows for adaptation depending on the setting and the maternity care professionals involved to support the development of individual practice guidelines and institutional policies and procedures.
This document is specific to considerations regarding hydrotherapy during labor and/or birth and is provided as an educational aid to members of the endorsing organizations and interested maternity care providers. This model practice template is not intended to dictate an exclusive course of management or to substitute for individual professional judgment. It presents recognized methods and techniques of clinical practice that maternity care providers may consider incorporating into their practices. The needs of an individual client or the resources and limitations of a particular setting or type of practice may appropriately lead to variations in clinical care. The information in this document is gleaned from published literature available through April 2016. This document will be reviewed against newly available scientific evidence and/or every 5 years after initial publication.
ACKNOWLEDGEMENTS
This document was developed by a multi-organizational task force hosted by the American College of Nurse-Midwives. Members of the task force were self-identified experts in use of hydrotherapy, researchers who have addressed this topic, and formally appointed representatives from the participating organizations. The organizations formally endorsing this document include the American Association of Birth Centers, American College of Nurse-Midwives, Midwives Alliance of North American, and National Association of Certified Professional Midwives. Contributing authors to this document include the following individuals:
Lisa Kane Low, CNM, PhD, FACNM, FAAN
Associate Professor, University of Michigan School of Nursing
President, American College of Nurse-Midwives
Elizabeth Nutter, CNM, DNP
Major, United States Army
Representative, American College of Nurse-Midwives
Colleen Donovan-Batson, MS, CNM, ARNP
Director, Division of Health Policy and Advocacy
Midwives Alliance of North America
Cynthia B. Flynn, CNM, PhD, FACNM
Representative, American Association of Birth Centers
Lesley Meenach Rathbun, CNM, FNP, MSN
Director, Charleston Birth Place
President, American Association of Birth Centers
Maria Christina Johnson, CNM, MS, FACNM
Director of Professional Practice and Health Policy
American College of Nurse-Midwives National Office Staff
Kaye Kanne, CPM
Representative, National Association of Certified Professional Midwives
Jenna Shaw-Battista, CNM, PhD, FACNM
Representative, American College of Nurse-Midwives
[Corrections added after online publication November 29, 2016: For Colleen Donovan-Batson: Name and credentials were corrected from “Colleen Batson-Donovan, CPM” to “Colleen Donovan-Batson, MS, CNM, ARNP” and “Public” was removed from the title. For Lesley Meenach Rathbun: Rathburn was corrected to Rathbun.]
Individual Expert Contributors
Roma Allen, MSN, RNC-OB
Carrie F. Bonsack, CNM, DNP
Shaunti Meyer, CNM, MA, MS
Catherine Ruhl, CNM, MSN
Wednesday, 06 July 2022
Oxford Brookes University
New analysis of research shows that using a birth pool during labour provides “clear benefits” for healthy mums and their newborn, with less intervention and fewer complications during and after the birth than when compared to labouring and giving birth on land. Mothers also report higher levels of satisfaction with their birth experience.
Dr Ethel Burns of Oxford Brookes University Faculty of Health and Life Sciences led a team of researchers, working with Dr Claire Feeley (Oxford Brookes), Dr Priscilla Hall (Emory University, USA) and Dr Jennifer Vanderlaan (University of Nevada, USA). The research looking at 157,546 sets of mothers and babies was published today, in the journal BMJ Open .
What is water immersion during labour?
Water immersion in a birth pool during labour and birth can be divided into two distinct but overlapping categories. Some women may choose to leave a birth pool before giving birth, and others remain in the birth pool to give birth. The researchers wanted to compare healthcare interventions during labour and birth between water birth, labouring in water, and standard care with no water immersion.
The research which was reviewed as part of the study included a broad range of interventions and outcomes. These included things like what drugs were given to ease pain, the health of the baby at birth, loss of blood after the baby was born and the condition of mother and baby.
Low tech care option
Dr Ethel Burns, Senior Midwifery Lecturer at Oxford Brookes University said: ”This research shows that it is just as safe for healthy mothers to give birth in water as on land and that there are considerable benefits for mothers who choose to labour in a birthing pool. Water immersion is an effective method to reduce pain in making it a low-tech way to improve care quality and mothers’ satisfaction with care”.
The authors recommended that future research should include factors that are known to influence interventions and outcomes during and after labour or birth such as how many children a woman has already had, where she gives birth, who looks after her, and the care she receives.
Prospective cohort study of water immersion for labour and birth compared with standard care in an Irish maternity setting
Paula L Barry, Lean E McMahon, Ruth AM Banks, Ann M Fergus, Deirdre J Murphy
Abtract:
Objective To examine the birth outcomes for women and babies following water immersion for labour only, or for labour and birth.
Design Prospective cohort study.
Setting Maternity hospital, Ireland, 2016–2019.
Participants A cohort of 190 low-risk women who used water immersion; 100 gave birth in water and 90 laboured only in water. A control group of 190 low-risk women who received standard care.
Methods Logistic regression analyses examined associations between water immersion and birth outcomes adjusting for confounders. A validated Childbirth Experience Questionnaire was completed.
Main outcome measures Perineal tears, obstetric anal sphincter injuries (OASI), postpartum haemorrhage (PPH), neonatal unit admissions (NNU), breastfeeding and birth experiences.
Results Compared with standard care, women who chose water immersion had no significant difference in perineal tears (71.4% vs 71.4%, adj OR 0.83; 95% CI 0.49 to 1.39) or in OASI (3.3% vs 3.8%, adj OR 0.91; 0.26–2.97). Women who chose water immersion were more likely to have a PPH ≥500 mL (10.5% vs 3.7%, adj OR 2.60; 95% CI 1.03 to 6.57), and to exclusively breastfeed at discharge (71.1% vs 45.8%, adj OR 2.59; 95% CI 1.66 to 4.05). There was no significant difference in NNU admissions (3.7% vs 3.2%, adj OR 1.06; 95% CI 0.33 to 3.42). Women who gave birth in water were no more likely than women who used water for labour only to require perineal suturing (64% vs 80.5%, adj OR 0.63; 95% CI 0.30 to 1.33), to experience OASI (3.0% vs 3.7%, adj OR 1.41; 95% CI 0.23 to 8.79) or PPH (8.0% vs 13.3%, adj OR 0.73; 95% CI 0.26 to 2.09). Women using water immersion reported more positive memories than women receiving standard care (p<0.01).
Conclusions Women choosing water immersion for labour or birth were no more likely to experience adverse birth outcomes than women receiving standard care and rated their birth experiences more highly.
Waterbirth: a national retrospective cohort study of factors associated with its use among women in England
H. Aughey,J. Jardine,N. Moitt,K. Fearon,J. Hawdon,D. Pasupathy,I. Urganci,NMPA Project Team &T. Harris
BMC Pregnancy and Childbirth volume 21, Article number: 256 (2021)
Abstract
Background
Waterbirth is widely available in English maternity settings for women who are not at increased risk of complications during labour. Immersion in water during labour is associated with a number of maternal benefits. However for birth in water the situation is less clear, with conclusive evidence on safety lacking and little known about the characteristics of women who give birth in water.
This retrospective cohort study uses electronic data routinely collected in the course of maternity care in England in 2015–16 to describe the proportion of births recorded as having occurred in water, the characteristics of women who experienced waterbirth and the odds of key maternal and neonatal complications associated with giving birth in water.
Methods
Data were obtained from three population level electronic datasets linked together for the purposes of a national audit of maternity care. The study cohort included women who had no risk factors requiring them to give birth in an obstetric unit according to national guidelines. Multivariate logistic regression models were used to examine maternal (postpartum haemorrhage of 1500mls or more, obstetric anal sphincter injury (OASI)) and neonatal (Apgar score less than 7, neonatal unit admission) outcomes associated with waterbirth.
Results
46,088 low and intermediate risk singleton term spontaneous vaginal births in 35 NHS Trusts in England were included in the analysis cohort. Of these 6264 (13.6%) were recorded as having occurred in water. Waterbirth was more likely in older women up to the age of 40 (adjusted odds ratio (adjOR) for age group 35–39 1.27, 95% confidence interval (1.15,1.41)) and less common in women under 25 (adjOR 18–24 0.76 (0.70, 0.82)), those of higher parity (parity ≥3 adjOR 0.56 (0.47,0.66)) or who were obese (BMI 30–34.9 adjOR 0.77 (0.70,0.85)). Waterbirth was also less likely in black (adjOR 0.42 (0.36, 0.51)) and Asian (adjOR 0.26 (0.23,0.30)) women and in those from areas of increased socioeconomic deprivation (most affluent versus least affluent areas adjOR 0.47 (0.43, 0.52)).
There was no association between delivery in water and low Apgar score (adjOR 0.95 (0.66,1.36)) or incidence of OASI (adjOR 1.00 (0.86,1.16)). There was an association between waterbirth and reduced incidence of postpartum haemorrhage (adjOR 0.68 (0.51,0.90)) and neonatal unit admission (adjOR 0.65 (0.53,0.78)).
Conclusions
In this large observational cohort study, there was no association between waterbirth and specific adverse outcomes for either the mother or the baby. There was evidence that white women from higher socioeconomic backgrounds were more likely to be recorded as giving birth in water. Maternity services should focus on ensuring equitable access to waterbirth.

Water birth pools serve a pivotal role in enhancing the experience of physiological labour and natural childbirth for mothers.
In fact, they are particularly effective in helping mothers manage pain without relying on analgesia for relief (National Institute for Health and Care Excellence, 2014).
Research has shown that women who enter a warm water pool during established labour are better equipped to cope with the pain associated with childbirth.

Immersion in warm water has been unequivocally proven to offer significant physiological and psychological benefits during labor (Cluett et al., 2004).
The benefits extend beyond pain management; women who choose water birth often report a heightened sense of fulfillment and accomplishment, while babies experience a gentler, less traumatic birth process (Royal College of Obstetricians and Gynaecologists, 2014).
In addition to these advantages for mothers and babies, midwives also experience increased job satisfaction, and healthcare facilities can save resources and costs by providing water birth options (National Institute for Health and Care Excellence, 2014).

Statistics from the National Maternity Survey in 2014 indicate that nearly a third of women in the UK benefited from using a water birth pool (Care Quality Commission, 2014).
With up to 60% of mothers showing interest in natural birth, it is opportune to consider expanding the availability of this safe, cost-effective approach (American College of Obstetricians and Gynecologists, 2017).
On dry land, mothers face the challenge of gravity, which limits their movement as labor progresses and fatigue sets in.

Many women may lack the physical fitness required to maintain upright postures for extended periods (Gupta et al., 2007).
Additionally, mothers who are overweight or obese may struggle to cope with the physical demands of labor (Vahratian et al., 2005).
The transition from land to water can rejuvenate and energize mothers, providing them with a newfound sense of purpose.

The buoyancy of water reduces a mother’s relative weight by approximately 33%, allowing her to move in ways that would be impossible on land and explore natural labor and birthing postures (American College of Nurse-Midwives, 2014).
Furthermore, the warm water’s calming and relaxing effects promote the release of oxytocin, a critical hormone in childbirth.
Oxytocin induces uterine contractions and triggers the “fetal ejection reflex,” further aiding the birthing process.

Immersion in water has been shown to have a positive physiological impact on hormone secretion, including oxytocin surges that can facilitate cervical dilation and stimulate contractions (Odent, 2014).
In conclusion, water birth pools offer a multifaceted approach to childbirth that benefits both mothers and babies, enhances midwives’ job satisfaction, and provides cost-effective options for healthcare facilities.
The evidence supports the integration of water birth as a valuable and safe method to promote natural childbirth and physiological labor experiences.
Feeling relaxed, secure and in control and being able to move about freely can make
it more likely for you to have a quicker and more natural birth.
For some women using a birthing pool can offer all of these benefits.
Today more and more women are considering using water for pain relief in labour.
A midwife can support you in using a birthing pool at home or in our midwife-led units
at Colchester General Hospital and Clacton and Harwich hospitals in the community.
Using a birthing pool is likely to increase the chances of a normal vaginal delivery
and therefore we would like to offer this option to as many women as possible.
We have compiled this leaflet to give you and your partner relevant information about
labouring and giving birth in water.
Please talk to your midwife during the antenatal period who will be able to answer any questions you may have.
Please click here to read the full document
Background: For women at low risk of childbirth complications, water immersion during labour is a care option in many high income countries.
Our aims were (a) to describe maternal characteristics, intrapartum events, interventions, maternal and neonatal outcomes for all women who used a birthing pool during labour who either had a waterbirth or left the pool and had a landbirth, and for the subgroup of women who had a waterbirth in 19 obstetric units, and (b) to compare maternal characteristics, intrapartum events, interventions, and maternal and neonatal outcomes for women who used a birthing pool with a control group of women who did not use a birthing pool for whom we prospectively collected data in a single centre.
Methods: Prospective observational study in 19 Italian obstetric units 2002-2005.
Participants were: (a) 2,505 women in labour using a birthing pool in 19 obstetric units; and (b) 114 women in labour using a birthing pool and 459 women who did not use a birthing pool in one obstetric unit.
Descriptive statistics were calculated for the sample as a whole and, separately, for those women who gave birth in water. Categorical data were compared using Chi square statistics and continuous data by T-tests.
Results: Overall, 95.6% of women using a birthing pool had a spontaneous vertex delivery, 63.9% of which occurred in water. Half of nulliparas and three quarters of multiparas delivered in water.
Adverse maternal and neonatal outcomes were rare.
There were two cases of umbilical cord snap with waterbirth.
Compared with controls, significantly more women who used a birthing pool adopted an upright birth position, had hands off delivery technique, and a physiological third stage.
Significantly fewer nulliparas had an episiotomy, and more had a second degree perineal tear, with no evidence of a difference for extensive perineal tears.
Conclusions: Birthing pool use was associated with spontaneous vaginal birth.
The increase in second degree tears was balanced by fewer episiotomies.
Undue umbilical cord traction should be avoided during waterbirth.
Click here for PDF of the study
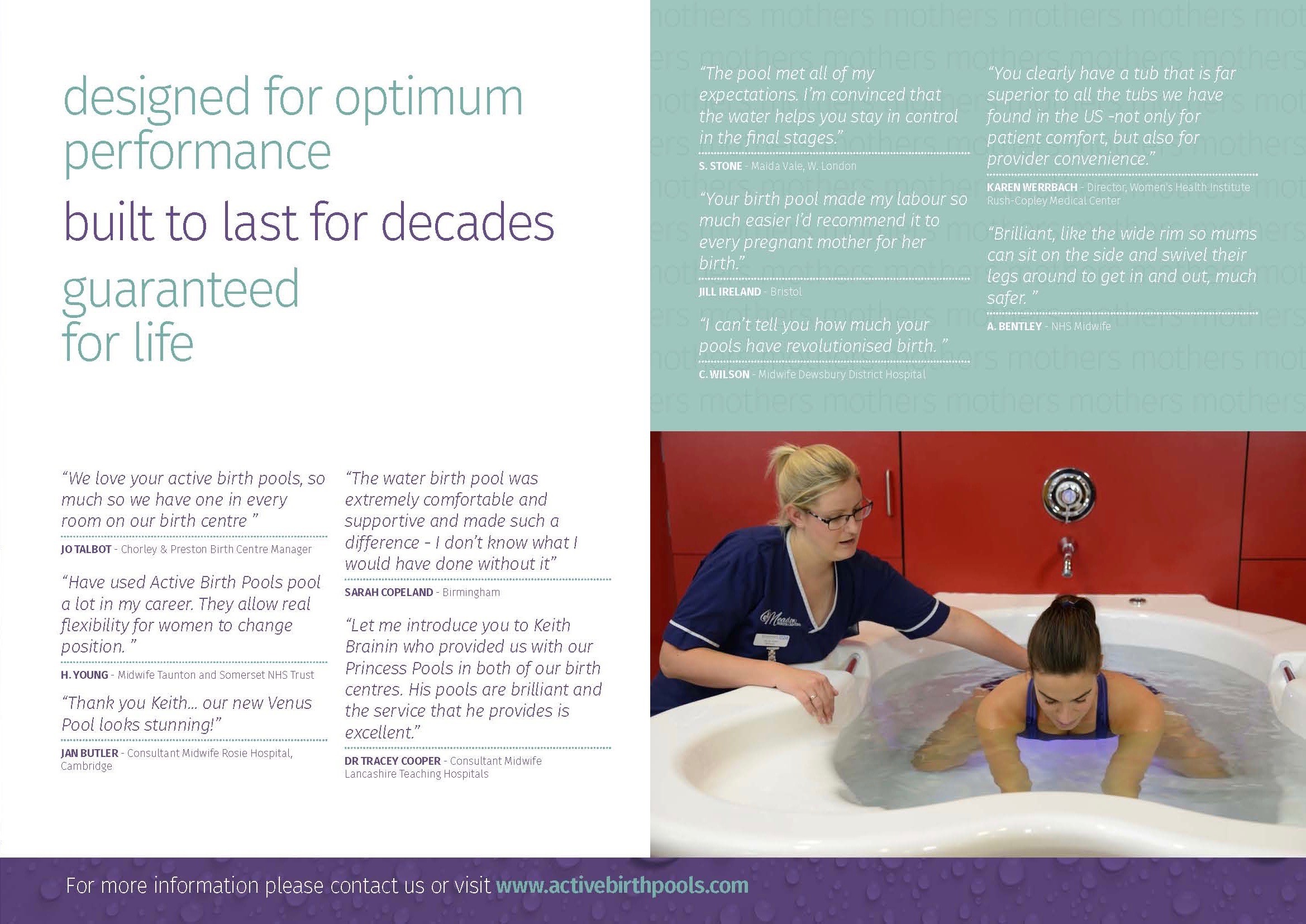
Background: Water immersion during labour can provide benefits including reduced need for regional analgesia and a shorter labour.
However, in the United Kingdom a minority of women use a pool for labour or birth, with pool use particularly uncommon in obstetric-led settings.
Maternity unit culture has been identified as an important influence on pool use, but this and other possible factors have not been explored in-depth.
Therefore, the aim of this study was to identify factors influencing pool use through qualitative case studies of three obstetric units and three midwifery units in the UK.
Methods: Case study units with a range of waterbirth rates and representing geographically diverse locations were selected. Data collection methods comprised semi-structured interviews, collation of service documentation and public-facing information, and observations of the unit environment.
There were 111 interview participants, purposively sampled to include midwives, postnatal women, obstetricians, neonatologists, midwifery support workers and doulas.
A framework approach was used to analyse all case study data.
Results: Obstetric unit culture was a key factor restricting pool use.
We found substantial differences between obstetric and midwifery units in terms of equipment and resources, staff attitudes and confidence, senior staff support and women’s awareness of water immersion.
Generic factors influencing use of pools across all units included limited access to waterbirth training, sociodemographic differences in desire for pool use and issues using waterproof fetal monitoring equipment.
Conclusions: Case study findings provide new insights into the influence of maternity unit culture on waterbirth rates.
Access to pool use could be improved through midwives based in obstetric units having more experience of waterbirth, providing obstetricians and neonatologists with information on the practicalities of pool use and improving accessibility of antenatal information.
In terms of resources, recommendations include increasing pool provision, ensuring birth room allocation
Click here for PDF of the study
Background: There is limited research examining midwives’ education, knowledge and practice around immersion in water for labour or birth. Our aim was to address this gap in evidence and build knowledge around this important topic.
Methods: This mixed method study was performed in two phases, between August and December 2016, in the birth centre of a tertiary public maternity hospital in Western Australia.
Phase one utilised a cross sectional design to examine perceptions of education, knowledge and practice around immersion in water for labour or birth through a questionnaire.
Phase two employed a qualitative descriptive design and focus groups to explore what midwives enjoyed about caring for women who labour or birth in water and the challenges midwives experienced with waterbirth.
Frequency distributions were employed for quantitative data. Thematic analysis was undertaken to extract common themes from focus group transcripts.
Results: The majority (85%; 29 of 34) of midwives surveyed returned a questionnaire.
Results from phase one confirmed that following training, 93% (27 of 29) of midwives felt equipped to facilitate waterbirth and the mean waterbirths required to facilitate confidence was seven.
Midwives were confident caring for women in water during the first, second and third stage of labour and enjoyed facilitating water immersion for labour and birth.
Finally, responses to labour and birth scenarios indicated midwives were practicing according to state-wide clinical guidance.
Phase two included two focus groups of seven and five midwives.
Exploration of what midwives enjoyed about caring for women who used water immersion revealed three themes: instinctive birthing; woman-centred atmosphere; and undisturbed space.
Exploration of the challenges experienced with waterbirth revealed two themes: learning through reflection and facilities required to support waterbirth.
Conclusions: This research contributes to the growing knowledge base examining midwives’ education, knowledge and practice around immersion in water for labour or birth.
It also highlights the importance of exploring what immersion in water for labour and birth offers midwives, as this research suggests they are integral to sustaining waterbirth as an option for low risk women.
Click here for PDF of the study
