Educational videos by midwives for midwives
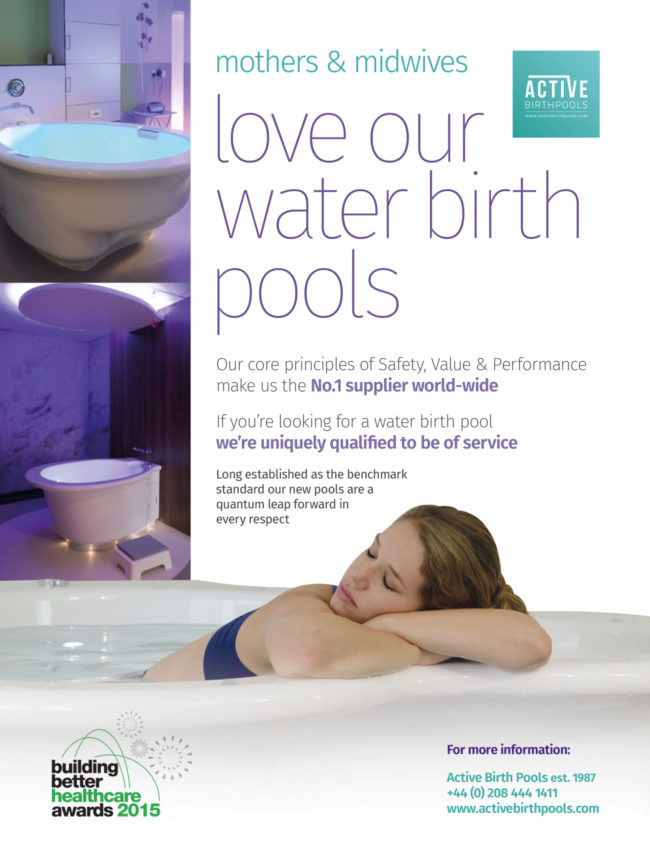
Category: Mothers and Midwives
Water safety and infection control risks you should know about before choosing a birth pool
Purchasing a water birth pool is a big responsibility.
Not only must financial considerations be taken into account, but more importantly Health and Safety risks.
There are other manufacturers who produce water birth pools that are safe but, many water birth pools are equipped with features that at first might seem safe or even an advantage, but in reality present risks or breach regulations.
These water birth pools (mainly produced in Europe) are over engineered and equipped with a profusion of fittings and features that put mothers and midwives at risk.
(We’re not showing images of other birth pools to illustrate the points below as this could be contentious.)

This whirlpool bath clearly shows a large number of unsafe fittings and systems as applied to water birth pools.
Note the overflow drain, recirculating water system, Swan neck tap, integral shower, rim mounted plumbing and controls
Because they are mounted on the pool, close to the water the potential for pool mounted fixtures and fittings to become contaminated with bacteria and cross infect is greatly increased.
Rim Mounted Taps and Spouts
Rim mounted taps, spouts and showers are one the biggest Health and Safety risks
These fittings present a serious infection control risk as the space between the surface of the pool and the fitting is a suitable breeding ground for bacteria.
Remember – bacteria are microscopic – even though the fitting may appear flush to the surface of the pool there is space for micro-organisms to establish themselves.
The risk that bacteria will propagate in the moisture between the plate and the rim is unacceptable.
There is also a risk that rim mounted taps could be contaminated with water from the pool and flow back into the tap.
There is the potential for back contamination of the tap, with bacterial colonisation into the system in contravention of water fitting regulations
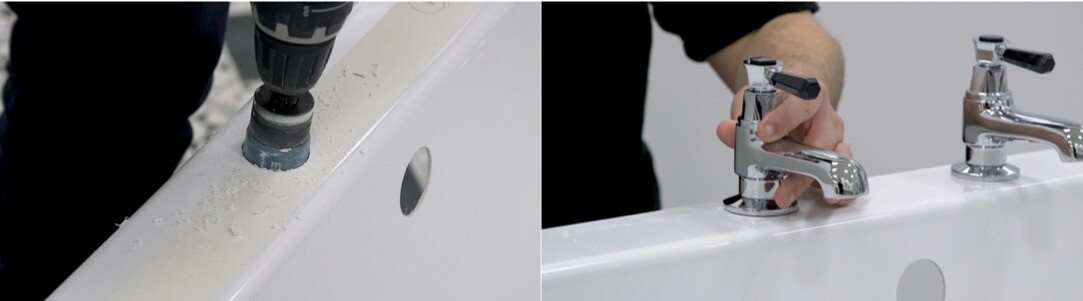
Taps and spouts for water birth pools should be wall mounted 25cm above the pool and fitted with back flow protection as shown in the photo of the Active II Water Birth Pool below:

Surface Mounted Hand Grips (internal and rim mounted)
Surface mounted handgrips are a serious infection control and manual handling risk.
Some water birth pools feature surface mounted hand grips similar to the ones shown above.
The is great potential for bacteria to become established between the fitting and the pool which makes these fittings an unacceptable infection control risk.
The risk of cross-infection is dramatically increased with surface mounted metalwork that is inside the pool as they come into direct contact with the water while the mother is using the pool.
From a manual handling perspective these handgrips are dangerous as they form an obstruction that mothers can hurt themselves on and they interfere with movement around the pool.

Swan Neck Taps
Swan neck taps are often seen mounted on the rims of water birth pools. Though attractive this type of tap presents a significant infection control risk.
Swan neck taps retain larger volumes of water which then stagnates and HFN 30 and HPSC recommends that swan-neck taps should not be used.
This is because they do not empty after use and could be prone to microbial biofouling with microorganisms including Legionella and P. aeruginosa the latter of which was associated with a swan neck tap during the neonatal outbreak in Northern Ireland (HPSC, 2015).

Re-circulating water systems
Re-circulating or pumped systems with jets such as whirlpools and jacuzzi present the perfect conditions for the growth of micro-organisms.
Water systems like these present the highest levels of risk as they produce aerosols.
Aerosols are generated when the water surface is broken – for example, by falling water droplets, splashing, or by bubbles breaking at the surface.
Once introduced to these systems, Legionella and Pseudomonas thrive and can become aerosolised and then inhaled.
Integral Plumbing Systems
Plumbing systems like these utilise flexible and non-flexible piping, overflow drains, handheld showers, pumps, hoses, heaters, surface mounted fittings and filters.
These systems are impossible to clean, disinfect or monitor and therefore present an extremely high Infection Control Risk.
Stagnant water within the system is an ideal breeding ground for bacteria.
UK regulations state that water birth pools fitted with thermostatically controlled mixer taps plumbed directly into the hospitals water supply.
Hand held showers
Handheld showers present a significant infection control risk.
If the shower head falls in the pool it may be contaminated with bacteria that could breed and be passed on next time the shower is used.
Department of Health regulations clearly stipulate that handheld showers and bath/shower mixers are not installed for use with water birth pools as they present a Fluid Category 5 risk to the mains water supply.
N.B. There are systems available that enable you to detach the hose and shower head from the tap. These are permissible as long as the shower fittings are detached when the pool is in use and only employed afterwards for cleaning.
Integral Plumbing Systems
Plumbing systems like these utilise flexible and non-flexible piping, overflow drains, handheld showers, pumps, hoses, heaters, surface mounted fittings and filters.
These systems are impossible to clean, disinfect or monitor and therefore present an extremely high Infection Control Risk.
Stagnant water within the system is an ideal breeding ground for bacteria.
UK regulations state that water birth pools should be filled with wall mounted, thermostatically controlled mixer taps plumbed directly into the hospitals water supply.

Pumped heating systems
Heating systems for water birth pools are not necessary and present unacceptable infection control risks.
Water is pumped through a heat exchanger and then back into the pool creating the ideal environment for bacteria to breed.
These systems present one of the highest infection control risks and should not be utilised.
Bacteria filters and disinfection systems
Some water birth pools are equipped with these devices in an attempt to mitigate the risk of infection and bacteria infestation that are inherent in built-in plumbing systems.
Bacteria filters and disinfection systems can not be relied upon and will not guarantee adequate hygiene standards.
Overflow drains
Overflow drains harbour bacteria and can serve as a conduit for cross infection.
Regulations are very clear on this point.
Overflow drains should not be fitted to water birth pools as they constitute a constant infection control risk.

Surface mounted metalwork
Metalwork such as grab rails, taps and handles are an obstacle that comes between mother and midwife.
These fittings ALL present a serious infection control risk as the space between the surface of the pool and the fitting are perfect for bacteria.
Remember – bacteria are microscopic – even though the fitting may appear flush to the surface of the pool there is space for bacteria!

Doors
There is no reason for a water birth pool to have a door and many reasons why they should not.
Doors are mistakenly used for two reasons:
- To facilitate emergency evacuations
- To help mothers get in and out of the pool
Doors present an extremely high risk of infection and should be banned from use in water birth pools for this reason alone.
The door seal (typically foam or rubberised material) is the perfect breeding ground for bacteria.
From manual handling perspective doors are not practical or fit for purpose.
They actually complicate emergency evacuations and put mothers and midwives at risk.
Active Birth Pools: Water Safety, Hygiene and Infection Control
Superior material results in superior safety, value and performance
Winner – Building Better Healthcare Awards
At the ‘Building Better Healthcare’ awards ceremony the Active Birth Pool was highly commended in the award for best internal building product.
In their comments the judges praised the quality of our design and manufacturing process and went on to say that they found the Active Birth Pool very appealing.

All aspects of design, engineering and manufacture were focused on develop a water birth pool of unparalleled beauty, quality, functionality and durability that is backed by an extraordinary life-time year guarantee.
Foremost consideration was given to how mothers and midwives relate to and interact with the pool employing ergonomic principles to design for the interaction and dynamic at play.
Mothers have the space to move freely and comfortably and are supported in the postures natural to a physiological labour and birth.

The “signature” extra-wide rims with broad “bull-nosed” shaped edges flowing into the skirting panel and down to the floor are an important feature of the Active Birth Pool that sets it apart.
The wide flat rim allows mothers to lean forward, resting on their forearms in comfort – one of the most natural and effective positions during labour.
It provides secure, safe, stable support for women to enter and leave the pool and for midwives and partners to lean or rest on while attending the mother.
The handrails, which are set into the profile of the rim, provide perfect support for the mother in upright positions.

The critical issue of emergency evacuation has been resolved by incorporating features into the pool to give midwives several options for evacuating the mother that are in compliance with Health & Safety and Manual Handling regulations.
The Labour Support and Safety Seats are distinguishing features of the Active Birth Pool
1) This physiologically designed labour support seat has proven to help the mother’s pelvis and birth canal open in preparation for a natural, physiological birth.
2) The distinctive rim level safety seat provides a wide comfortable platform for the mother to lean on, a safe means for emergency evacuation and is ideal for midwives to monitor the mother without her having to stand up or leave the pool.

The unique seamless one-piece construction incorporates a deeply sculpted concave skirting panel to allow midwives to work in comfort with their legs well under the pool.
The new Active Birth Pool is fabricated in Ficore® composite, a proprietary material that was specially developed for baths and designed to negate the risk of problems associated with other materials.
Ficore is 50% harder than acrylic and fibreglass (which other birth pools are made from) and highly resistant to chemicals.
Despite the rigidity and hardness of the surface it is extremely smooth, tactile and warm to the touch.
Its high insulation factor enables the Active Birth Pool to maintain its temperature up to six times longer than standard acrylic or fibreglass birth pools.

To help mothers control, define and personalise the delivery room, the Active Birth Pool is equipped with multi-colour chromotherapy LED lighting and integral bluetooth sound.
Our ingenious Integral Bluetooth Sound System allows the mother to wirelessly connect her phone and listen to the music of her choice.
Two integral speakers turn the birth pool into a highly refined audio loudspeaker.
When you examine the new Active Birth Pool you’ll immediately notice the superior finish and signature design elements.
Look a little closer and the quality of the components such as the drainage system, the support structure that underpins the pool, the fittings on the access panel, the lighting system, handrails and metal work becomes apparent.

If you are looking for a water birth pool to install in a maternity unit the incomparable new Active Birth Pool should be your first choice.
Handmade and custom built to order by a team who together have over 95 years experience in the design and production of high-end baths the new Active Birth Pool will provide decades of service and be an invaluable aid to mothers who want to have a natural birth.
The Active Birth Pool conforms to regulations issued by the Department of Health and the guidelines set forth in the Water Birth Safety Initiative.
Introducing the Active II Water Birth Pool: Enhancing Maternity Care with Advanced Design
Note: this article taken from “Building Better Healthcare” magazine – November 2015
Guidelines: Getting in and out of the pool
The simple act of getting into the pool is one of the most misunderstood aspects relating to the use water birth pools.
The truth is that multi-step units are dangerous and in the case of Active Birth Pools unnecessary as the video below clearly demonstrates.
Health and Safety and Manual Handling experts strongly advise against the use of multi-step units as they present unacceptable safety risks.
They say that, “mothers in strong labour should not climb up and over the rim of the pool and down onto a submerged plinth because it is not safe or practical”.
In addition these bulky step unit take up too much space, obstruct movement around the pool and are a trip hazard.

With the help of Manual Handling and Ergonomic Design experts we designed a simple, safe way for mothers to get into our pools.
The distinctive extra-wide, bull-nosed shaped rim is relatively low making it perfect for mothers to sit on and gently swivel into the water.
There is no climbing – mothers are grounded at all times and safeguarded from risk.

All women no matter what their shape or size will find it exceptionally easy to get into our pools.
Mothers don’t even think about it – they move instinctively and naturally lower themselves into the water.
And midwives will be safeguarded from the risk associated with physically supporting mothers as they climbs up the steps .

To put this in perspective:
The average height of our pools is 75cm – about the same height as a desk or dining table.
Our 15cm high single step makes the height of the pool 60cm – the same height as an ordinary bathtub.
You don’t need a big step unit to get into your bath at home, do you?

The keyword that defines our design ethos is Active.
The keyword that defines our approach to design is ‘Active’.
If we look up the definition of ‘Active Birth’ we get, “Childbirth during which the mother is encouraged to move around freely and assume any position which feels comfortable”.
Active Birth Pools provide mothers with the space and depth to move freely in the postures natural to labour and birth.
As she moves, she intuitively discovers features that provide support and make her more comfortable.

Design is based upon the dynamics of mothers and midwives as they interact with the pool and each other.
Form is based on function and pared down to the essence of aesthetic utility.
There is a reason for every shape, every curve and every form.

Our water birth pools encourage mothers to move freely and naturally.
They instinctively interact with the pool and find comfort and support wherever they are.
Freedom of movement combined with the relaxing effects of warm water and release of oxytocin significantly increases the possibility of physiological labour and birth.

We are pioneers, innovators and trend setters.
Our water birth pools have continuously evolved over the past 35 years.
We’re able to achieve our latest designs because of the highly specialised material we use.
Ficore, a composite resin with unique properties enables us to create incredibly curvaceous pools that mothers and midwives find exceptionally comfortable, practical and easy to use.

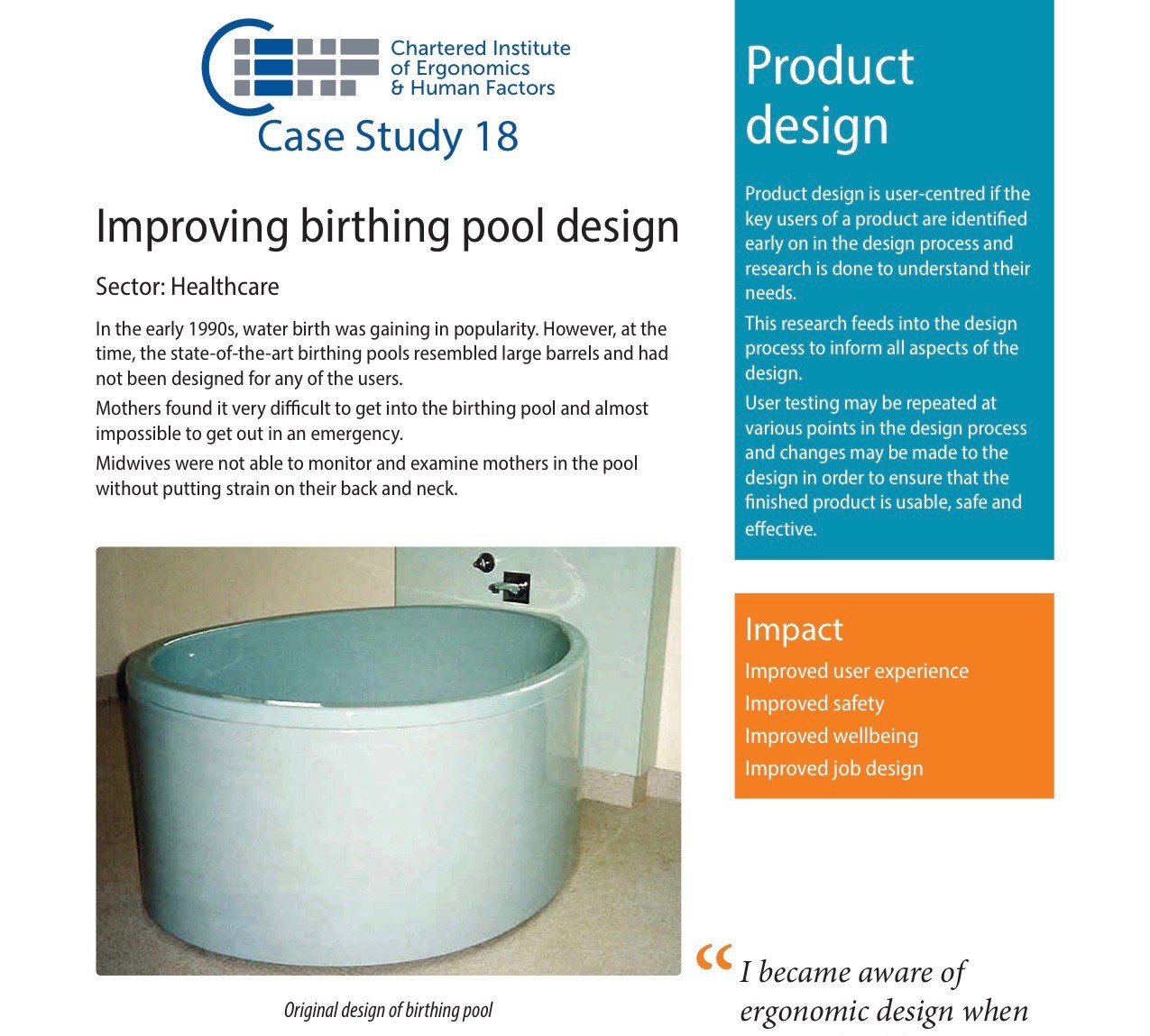
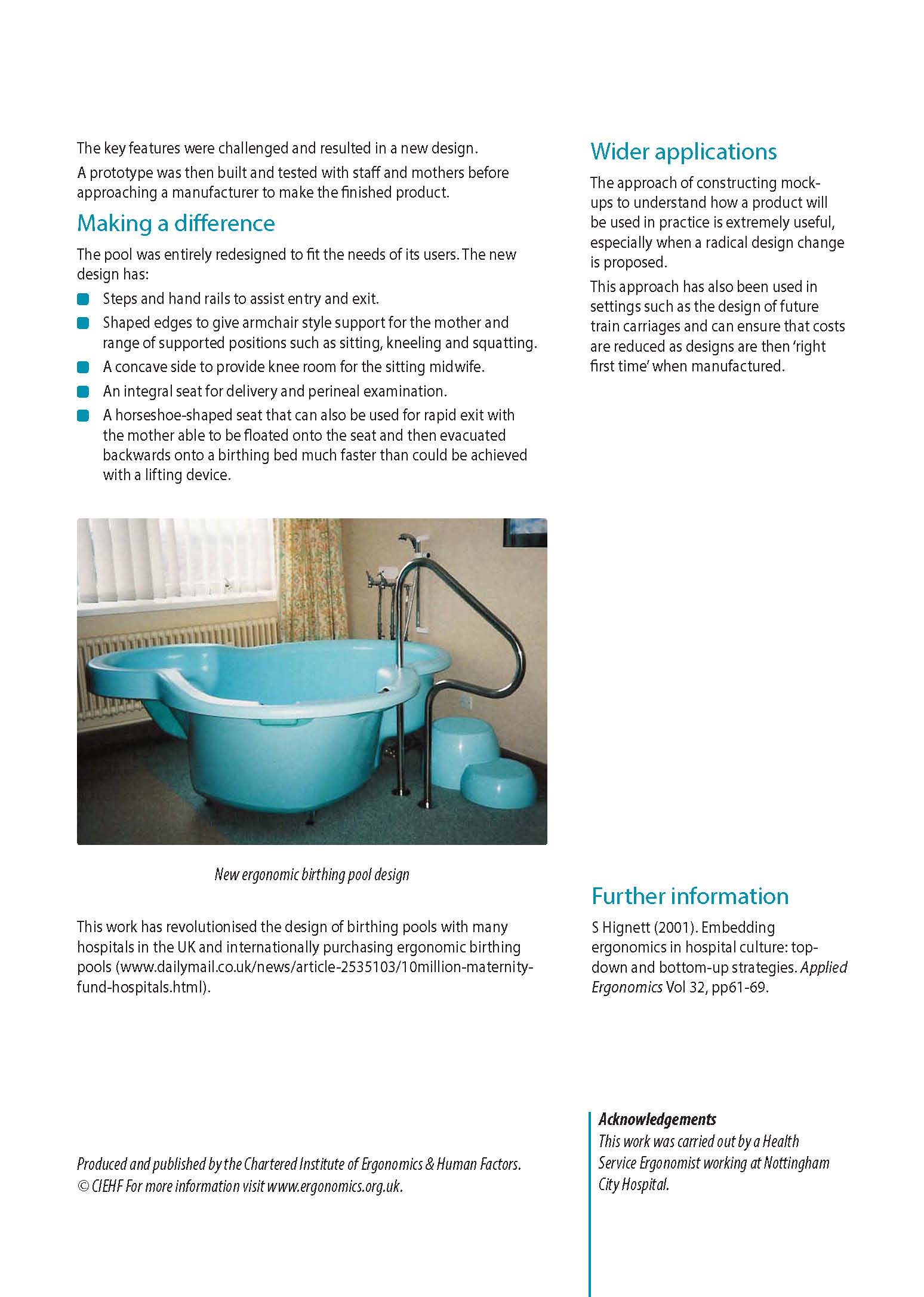
In mid-90’s we met with a design specialist to discuss ways our water birth pools could be improved to better serve the needs of mothers and midwives.
This lead to the ground-breaking innovations in birth pool design that have culminated in todays range of award winning water birth pools.
Below a copy of article that appeared in the Chartered Institute of Ergonomics and Human Factors charting the paradigm shift in birth pool design that occurred in the mid-90’s:
See our water birth pools in your delivery room
Would you like to see how our water birth pools would look in your delivery room?
Simply use your phone or tablet and click on this link:
Hint: its best to clear the space of all movable objects before using the 3D Viewer to get a realistic image of what it will look like in situ.
The Benefits of Labouring in Water for Plus-Size Women
Childbirth is a transformative experience, and every expectant mother deserves the opportunity to have a comfortable and empowering birthing experience.
For plus-size women, the challenges of labour and delivery can sometimes be compounded by their body size.
However, one increasingly popular option that offers numerous benefits is labouring in water.
This article explores the advantages of water labour specifically for plus-size women, highlighting how it can enhance their birthing experience and overall well-being.

Buoyancy and Weight Support
One of the primary benefits of labouring in water for plus-size women is the buoyancy and weight support provided by the water.
As water buoys the body, it reduces the gravitational pull on joints and muscles, making it easier for women with larger body sizes to move and change positions during labour.
This buoyancy can alleviate the pressure on the pelvis and lower back, which is especially important for plus-size women who may already experience discomfort in these areas due to their size.
Reference: Geissbuehler V, Stein S, Eberhard J. Waterbirths compared with land births: an observational study of nine years. J Perinat Med. 2004;32(4):308-314.
Pain Relief and Relaxation
Warm water has a natural analgesic effect, helping to ease the pain and discomfort associated with labour contractions.
Plus-size women may have additional challenges due to their size, such as increased strain on the body, making the soothing properties of water particularly beneficial.
Water labour can promote relaxation, reduce stress, and create a calming environment, allowing mothers to focus on their breathing and coping techniques.
Reference: Harper SG, Lynch M, Vernacchio L. “Waterbirth: a retrospective comparative study of waterbirth and land birth outcomes.” Journal of Perinatal Education. 2002;11(2):22-29.

Improved Blood Circulation
For plus-size women, carrying extra weight can sometimes lead to issues with blood circulation and swelling in the extremities.
Immersing in warm water during labour can improve blood circulation by promoting vasodilation, which can help reduce swelling and alleviate discomfort.
Improved circulation can also support the baby’s oxygen supply during contractions.
Reference: Mollamahmutoglu L, Moraloğlu Ö, Ozyer S, et al. Warm showers as an alternative to warm sponges for the management of third stage of labour. European Journal of Obstetrics & Gynaecology and Reproductive Biology. 2002;101(1):19-23.
Enhanced Mobility and Positioning
Water labour allows for greater freedom of movement, which is especially valuable for plus-size women.
The buoyancy of water makes it easier to change positions, squat, or kneel, providing a range of options for comfort and facilitating the progress of labour.
The flexibility to find a comfortable position can be especially important for plus-size women, as it may help prevent complications and reduce the need for interventions.
Reference: Cluett ER, Burns E. Immersion in water in labour and birth. Cochrane Database of Systematic Reviews. 2009(2):CD000111.

Reduced Stress on Joints
The extra weight carried by plus-size women can put strain on their joints and ligaments, potentially leading to discomfort during labour.
Immersion in water can reduce the stress on joints, making movements smoother and less painful.
This can be particularly advantageous during the pushing phase of labour, as it allows for better control and coordination of efforts.
Reference: Zanetti-Daellenbach R, Tschudin S, Zhong X, et al. Influence of immersion in water on uterine contractility and cerebral oxygenation during the first stage of labour. Am J Obstet Gynecol. 2007;196(5):468.e1-8.
Conclusion
Laboring in water offers numerous benefits to plus-size women, enhancing their birthing experience and promoting a sense of empowerment during childbirth.
The buoyancy and weight support of water, coupled with its pain-relieving properties and improved circulation, make it a valuable option for managing the unique challenges associated with labouring while plus-size.
Ultimately, the decision to labour in water should be made in consultation with a healthcare provider, taking into account individual preferences and medical considerations.
Nevertheless, it’s clear that water labour can provide a positive and supportive environment for plus-size women, contributing to a more comfortable and fulfilling childbirth experience.
Active Birth Pools are designed to cater to the specific needs of plus-size women during childbirth
Our pools boast a spacious and ergonomic structure that allows for comfortable movement and positioning during labor.
Their wider dimensions and sturdy construction provide ample room and support for plus-size mothers, ensuring they can find comfortable birthing positions without constraints.
The carefully engineered design also takes into consideration accessibility, making it easier for expectant mothers of all sizes to enter and exit the pool safely.
These pools are equipped with features like grab rails and steps to ensure stability and ease of use.
In essence, the design of active birth pools prioritizes inclusivity and comfort, empowering plus-size women to have a positive and fulfilling birthing experience.
The Warm Embrace: How Warm Water in Water Birth Pools Facilitates the Release of Oxytocin
The use of water birth pools has gained popularity in recent years as expectant mothers seek alternatives that enhance the natural birthing experience.
One of the key factors contributing to the success of water births is the warm water in the birthing pool, creating an environment that encourages the release of oxytocin.
Often referred to as the “love hormone” or “bonding hormone,” oxytocin plays a crucial role in the progression of labour and the overall well-being of both mother and baby.

Understanding Oxytocin:
Oxytocin, produced by the hypothalamus and released by the pituitary gland, is a hormone known for its role in promoting social bonding, emotional connection, and uterine contractions during childbirth.
It is often associated with feelings of love, trust, and intimacy, and its presence is pivotal in the birthing process.
The Warm Water Effect:
Pain Relief and Relaxation: Warm water has inherent therapeutic properties, and when a laboring woman immerses herself in a water birth pool, the comforting embrace of warm water contributes to pain relief and relaxation.
The buoyancy of water alleviates the pressure on the body, reducing muscle tension and creating an environment conducive to calmness.
As the mother relaxes, the body is more apt to release oxytocin, facilitating the progression of labor.

Enhancing Blood Circulation:
The warm water in water birth pools promotes vasodilation, leading to improved blood circulation.
This enhanced blood flow is particularly beneficial during childbirth, as it ensures that the uterus receives an adequate supply of oxygen and nutrients.
The improved circulation helps in optimizing uterine contractions and, subsequently, the release of oxytocin.
Reducing Stress Hormones:
Warm water has a natural ability to decrease the production of stress hormones, such as cortisol.
By creating a serene and comfortable environment, the water birth pool minimizes the stress response, allowing the body to focus on the release of oxytocin.
This reduction in stress hormones supports a positive birthing experience and contributes to the mother’s overall well-being.

Facilitating the Bonding Process:
Oxytocin is not only crucial for uterine contractions but also plays a vital role in the bonding between mother and baby.
The warm water in the birthing pool promotes the release of oxytocin, fostering a sense of intimacy and connection between the mother and her newborn.
This early bonding experience can have lasting positive effects on the emotional well-being of both mother and child.
Promoting a Positive Birth Environment:
The warm water in water birth pools contributes to the creation of a positive and supportive birthing environment.
This positive ambiance, coupled with the physiological effects of warm water, enhances the mother’s overall experience, making her more receptive to the natural release of oxytocin.

Conclusion:
The warm water in water birth pools serves as a nurturing medium that promotes the natural release of oxytocin, enriching the childbirth experience for expectant mothers.
As healthcare providers and birthing centers continue to recognize the benefits of water immersion during labor, understanding the interplay between warm water and oxytocin release becomes essential.
By harnessing the therapeutic properties of warm water, the journey through childbirth becomes not only more comfortable but also profoundly connected, nurturing the beautiful bond between mother and baby.
Enhancing Midwifery Care: The Benefits of Water Birth Pools
Midwifery, a practice deeply rooted in supporting natural childbirth, has seen a remarkable evolution in the tools and techniques used to enhance the birthing experience.
Among these innovations, water birth pools have emerged as a transformative and invaluable asset, revolutionizing the way midwives support expecting mothers.
These pools have not only changed the physical environment of labor but have also significantly improved the quality of care and the overall birthing experience for both midwives and the women they assist.

Creating an Ideal Birthing Environment
Water birth pools provide a serene and calming setting, transforming the atmosphere of the birthing room.
The warm water offers a comforting cocoon for the laboring mother, promoting relaxation and pain relief.
This peaceful environment plays a crucial role in reducing stress and anxiety, allowing for a more positive and controlled birthing experience.

Benefits for Midwives
For midwives, these pools are more than just a different birthing option—they represent a valuable tool that enhances their ability to provide care.
Here’s how water birth pools make a difference for midwives:
- Comfort and Control: Water immersion helps facilitate mobility and positioning for the mother, making it easier for midwives to support her during labor. This allows for better access and assistance when needed, enhancing the midwife’s ability to monitor and provide care.
- Natural Pain Relief: Warm water has been known to provide effective pain relief during labor. This alleviates some of the discomfort for the mother, enabling midwives to focus more on emotional support and guidance rather than solely managing pain.
- Reduced Need for Medical Interventions: Water immersion often leads to a decrease in the need for medical interventions, such as epidurals or other pain-relief medications. Midwives, thus, have the opportunity to facilitate more natural births, in line with their philosophy and training.
- Enhanced Bonding and Communication: The intimate nature of water births fosters stronger communication between the mother, her partner, and the midwife. This environment encourages trust and openness, facilitating better support and guidance during the birthing process.
Challenges and Considerations
While the advantages of water birth pools for midwives are significant, challenges exist, including the need for proper training in water birth techniques and ensuring the safety and hygiene of the pool and its surroundings.
Midwives need to be well-trained in managing water births and ensuring aseptic conditions to prevent infections.

The Future of Midwifery with Water Birth Pools
The growing popularity of water birth pools in many birthing centers and even home births suggests a shift in how mothers choose to bring their child into the world.
This, in turn, influences the practice of midwifery.
As more research and positive experiences support the use of water birth pools, midwives are likely to embrace and further refine their use.
Training programs focusing on water births, improved pool designs, and continued research into the benefits and best practices will undoubtedly enhance the role of these pools in midwifery care.

Conclusion
Water birth pools have undeniably revolutionized the landscape of childbirth.
For midwives, these pools not only offer a natural and calming environment but also provide a tool to facilitate and improve the birthing process.
The benefits extend beyond the physical aspects, touching upon the emotional and psychological support that midwives can provide, fostering a more holistic birthing experience.
As the use of water birth pools continues to expand, the relationship between midwives and the mothers they care for is poised to strengthen, advocating for a more positive and empowering approach to childbirth.
Midwives prefer our water birth pools because they’re the most comfortable and easy to use
The benefits of using water for labour and birth are well known, here are the facts…
The benefits of using water for labour and birth are well known…

Here are the facts…
- Relaxing in a deep pool of warm water can be a wonderful aid in labour. It’s worth having a pool mainly for this reason.
- Using a birth pool helps mothers to manage pain in labour and considerably reduces the need for medical pain relief.
- The buoyancy of the water supports the mothers body weight allowing her to relax more easily and deeply. They can cope better with contractions and also rest more comfortably in between them.
- It’s easier to use upright or squatting positions and move freely from one position to another, than it is on land.
- Being in a birth pool gives mothers an increased feeling of privacy and security. This enhances the secretion of hormones which stimulate uterine contractions and act as natural pain killers and relaxants.
- Studies show that labours tend to be shorter overall when a woman enters the pool at around 5cms. dilation.
- Fewer women need the help of obstetric interventions.

Women who receive less medical intervention generally stay in hospital for a shorter period of time.
The combination of an intervention free birth – with a short hospital stay result in a better experience for mother and baby.
Hospital staff and resources can be employed more efficiently.
Importantly – this results in significant financial savings!
A birth pool is a simple, inexpensive piece of equipment that has a major impact on the the quality of care and cost of having a baby.
Click here to learn more about our water birth pools and find out how they will deliver for you.

Water Birth Safety Initiative
Hospitals in the United Kingdom began allowing women to use specially designed pools of water for labour and birth during the 1980’s.
The wide-spread popularity and acceptance of water birth pools as a standard part of the maternity care package necessitated the development of guidelines & regulations to define standards and ensure they’re met.

The United Kingdom Department of Health has published a panoply of water safety directives that apply to water birth pools.
Policies and recommendations set forth in the Water Birth Safety Initiative are based upon these publications.
The Water Birth Safety Initiative (WBSI) calls for development of international standards modelled on the UK’s so that women the world over can benefit from the use of water for labour and birth safeguarded from risk.
The WBSI calls for the implementation of stricter protocols and sets forth recommendations for equipment standards.
The guidelines set forth in the WBSI are intended to serve as a framework of standards for birth pool suppliers, hospitals and midwives to work with to establish safe codes of practice.

Guidelines for Water Birth Pools Installed in Hospital
Water is more prone to bacteria growth after it leaves the public water distribution system and enters a building’s plumbing.
There it finds warmer temperatures, stagnation, and smaller pipes, valves and fittings.
Biofilm that forms on valves and fittings and pipe walls not only feeds bacteria but also protects them from the hot water and chlorine that typically would kill free-floating organisms.
Large systems with complex piping networks — like those found in hospitals, hotels and large apartment buildings — are especially prone to bacteria growth.15
Water Birth Pools that are installed in hospitals have the benefit of being maintained by staff to ensure that protocols are established, met and maintained.
Consideration and due diligence with regard to the prospective purchase of water birth pools and the assessment of pools already in use needs to be taken to ensure that the associated plumbing and electrical systems meet relevant safety standards.
The United Kingdom’s Department of Health and National Health Service has an exemplary safety record achieved by establishing rigorous sets of guidelines and regulations for the design, installation, use and maintenance (cleaning/disinfection) of water birth pools.
In the UK water birth pools are classed as a Category Fluid 5 water risk which represents a serious health hazard due to the concentration of pathogenic organisms, radioactive or very toxic substances, e.g. containing faecal material or other human waste; butchery or other animal waste or pathogens.
Water Birth Pools must be installed in compliance with water regulations as set forth in The Water Supply (Water Fittings) Regulations 1999.11

The 7 sins of water safety
To ensure high standards are met it is strongly advised that you do not use a water birth pool that has any of these features:
- Overflow drains
- Internal water inlets
- Hand-held showers
- Systems with flexible hoses or extended pipes
- Integral or secondary plumbing systems
- Any type of recirculating or pumped water systems such as whirlpool, jacuzzi, spa, bubbling, filtering etc
- Heating systems

1) Overflow drains
Overflow drains harbour bacteria and can serve as a conduit for cross infection.
Regulations are very clear on this point – overflow drains should not be installed on water birth pools as they constitute a constant infection control risk much more significant than the possible risk of damage due to water overflowing.11,12
Some digital taps on the market can be set for filling time thus obviating the risk of the pool overflowing.
2) Internal water inlets
Internal water inlets act in place of taps to fill the pool.
They are installed on the inside of the pool just above the water line and connected with pipework to a thermostatic valve.
If the water level rises there is a high risk of back flow enabling bacteria to enter the system creating a risk of cross infection.7
3) Handheld showers
Handheld showers present a significant infection control risk due to the fact that they can fall in the pool and be contaminated with bacteria that could breed and be passed on next time the shower is used.
Department of Health regulations clearly stipulate that handheld showers and bath/shower mixers are not installed for use with water birth pools. 13
Handheld showers present a Fluid Category 5 risk to the mains water supply.
It must not be possible to submerge the showerhead in the water due to risk of cross infection.
In order to comply with category 5 water regulations covering back siphonage, a class AUK3 air gap would be required, which generally prevents the use of handsets, unless there is a separate break tank installed in the hospital plumbing system.
4) Systems with flexible hoses or extended pipes
Systems that employ flexible piping, have branch pipes or hold stagnant water present a potential hazard and must not be used with water birth pools.
It is impossible to clean, disinfect or monitor these systems.
They have been proven to be a source of Legionella and Pseudomonas. 14
Weekly flushing recommendations recommended by the department of health cannot be executed with such systems, and the effectiveness of this cannot be monitored due to the inacessibility of the closed system.
5) Integral or secondary plumbing systems
Integral, secondary or proprietary plumbing systems are fitted to some water birth pools.
As these systems can employ flexible and non-flexible piping, overflow drains, handheld showers and are often pumped or recirculating they present a significant infection control risk and should be banned from use.
Regulations stipulate that water birth pools are filled from thermostatically controlled wall mounted mixer taps plumbed directly into the hospitals water supply with the minimum of pipework.
Not only do secondary or integral plumbing systems present unacceptable risks, they are impossible to clean, disinfect or monitor and therefore present an extremely high and unacceptable infection control risk.
They must not be present on pools used for labour and birth. 10
6) Recirculating or pumped water systems
Recirculating or pumped water systems such as whirlpool, jacuzzi, spa, bubbling, filtering etc. have the perfect environmental conditions to be a potential source for the growth of microorganisms, including legionella bacteria and must not be installed on water birth pools.
Water systems that are able produce aerosols represent the highest levels of risk.
Aerosols can be generated very easily when the water surface is broken -for example, by falling water droplets, splashing, or by bubbles breaking at the surface.
Once introduced to artificial water systems, Legionella can thrive in warm water (30 – 35 °C) and has been shown to be present on flexible seals and metal surfaces within plumbing systems used in domestic potable water supplies.
Inadequately maintained spa pools (birth pools with pumped or recirculating systems) provide ideal conditions to support the growth of legionellae and other microorganisms, which may then become aerosolised and subsequently inhaled.15

7) Heating systems
Heating systems for water birth pools are not necessary and present unacceptable infection control risks.7
There are two types of heating systems in use:
1. Recirculating system with a heat exchanger
Water is pumped out of the pool and through a heat exchanger and then flows back into the pool.
These systems present one of the highest infection control risks and should not be installed on a water birth pool under any circumstances. (covered by points 4, 5 and 6 above).
2. Electric heating systems
Similar to under floor heating found in homes do not present an infection control risk.
But, they do present an unacceptable health and safety risk and should therefore not be installed in water birth pools.
These systems consist of a network of cables embedded in the fabric of the birth pool that are attached to the power supply through a thermostat.
The heat is transmitted from the cables through the floor of the pool and then transferred to the water.
The inherent problem with these systems is that the water is relied on to take the heat away from the material.
If a woman remains motionless the heat becomes concentrated and a “hotspot” develops which can result in the woman being burned.

Recommendations
Plumbing for filling and emptying water birth pools should be simple, straight forward and kept to the minimum.
A set of taps (see below) mounted on the wall 15cm above the rim and a drainage system similar to that of a normal bath is all that is required.
Rim mounted taps present two areas of risk:
1. Women may hit their head on taps that are mounted on the rim of the pool causing injury.
In the throes of labour a woman is not as cognisant of her surroundings as she normally is.
She needs to be protected from the potential harm that could result from hitting her head or other part of her body on the spout.
2. Risk to the taps and pool caused by the labouring woman grabbing onto the spout for support could easily cause damage to the fitting or fabric of the pool.
Filling the birth pool
Water Birth Pools should be filled directly from the hospitals main water supply through a ¾ Thermostatic Mixing Valve (TMV).
To comply with UK National Health Service regulations the valve must have TMV3 approval for use in Healthcare and Commercial situations and certify that it conforms to the performance requirements of the Department of Health.16
To kill legionella and other bacteria, water in hospitals systems is heated to 60 – 80 °C.
Water temperature entering the birth pool should be limited by the TMV to 44 °C to prevent scalding.
The added benefit of using a TMV connected directly to the hospitals main water supply is that it can be set to automatically flush itself of stagnant water twice a day and be thermally disinfected periodically.

The use of a TMV ensures a safe water supply.
Digital thermostatic mixing valves with enhanced thermal performance that incorporate these features are ideal:
1) Programmable control to accurately mix and maintain the temperature of the water flowing into the birth pool and limit the temperature of the water to 44 °C to prevent scalding.17
2) Programmable fill duration to fill the pool to the desired depth and then turn off.
This is important as water birth pools are not allowed to have overflow drains installed and this feature will prevent the pool from overflowing when unattended.
3) Programmable duty flushing to ensure that water does not stagnate within the tap and associated pipe work, effectively controlling the multiplication of legionella & other bacteria in infrequently used outlets.
Flushing duration is in line with HSE L8 recommendations.18
4) Programmable high-temperature thermal disinfection to destroy the proteins in viruses and bacteria and render them as dead or inert.
Thermal disinfection works by achieving a moist heat which is set at a specific temperature for a set amount of time.
Viruses and bacteria are very sensitive to heat and they will die if exposed to higher temperatures. 19
Emptying the Pool
Water from a birth pool needs to be treated as Fluid category 5 waste representing a serious health hazard due to the concentration of pathogenic organisms derived from fecal material or other human waste and emptied directly into the hospital’s waste water system.20
The pipework needs to have a trap or U bend fit as close to the waste/drain as possible.
The drainage fitting or waste should seal neatly into the drain.
The drainage fitting should be cleaned and flushed through with disinfectant and then dried as part of the cleaning protocol.
The waste should be kept closed when the pool is not in use.
There should be NO flexible pipe used in the drainage pipework.21
The waste should be remotely operated (i.e. pop up waste with rim mounted control) and of the best quality, preferably high-grade brass, to resist the corrosive action of chlorides and other disinfectants.

End notes
The Water Birth Safety Initiative was conceived by Keith Brainin to motivate and enable birth pool suppliers and health care professionals to raise standards and implement protocols to make water birth safe.
References
[1] Healio – Infectious Disease News. (2014, December 26). Legionellosis death after water birth sparks call for stricter infection control protocols. http://www.healio.com/infectious-disease/practice management/news/online/%7Bfe352169-755d-4d21-9bb2-abb8ae209f89%7D/legionellosis-death-after-water-birth-sparks-call-for-stricter-infection-control-protocols
[2] Inquisitr. (2015, January 16). Oregon Water Birth Leaves Baby Disabled, Lawsuit Wants Labor Options Banned. http://www.inquisitr.com/1761136/oregon-water-birth-leaves-baby-disabled-lawsuits-wants-labor-options-banned/
[3] GOV.UK. Alert after Legionnaires’ disease case in baby, 2014. https://www.gov.uk/government/news/alert-after-legionnaires-disease-case-in-baby
[4] The Guardian. Legionnaires’ disease in baby is linked to heated birthing pool, June 17, 2014.http://www.theguardian.com/society/2014/jun/17/legionnaires-disease-heated-birthing-pool-baby-public-health
[5] Guidance from the Water Regulations Advisory Scheme (WRAS) https://www.wras.co.uk/consumers/advice_for_consumers/what_are_the_water_regulations_/
[6] M.W. LeChevallier, 2003 World Health Organization (WHO). Conditions favouring coliform and HPC bacterial growth in drinking- water and on water contact surfaces. Heterotrophic Plate Counts and Drinking-water Safety. Edited by J. Bartram, J. Cotruvo, M. Exner, C. Fricker, A. Glasmacher. Published by IWA Publishing, London, UK. ISBN: 1 84339 025 6.
[7] www.gov.uk. Public Health England advice on home birthing pools, 2014. https://www.gov.uk/government/news/public-health-england-advice-on-home-birthing-pools
[8] Health and Safety Executive. (2013). Legionnaires’ disease: Technical guidance [3.4], 2013. http://www.hse.gov.uk/pubns/priced/hsg274part3.pdf
[9] United Lincolnshire Hospitals NHS Trust UK. Cleaning, Disinfection and Sterilization Guidelines for Re-Usable Medical Devices 2010.
http://www.activebirthpools.com/wp-content/uploads/2014/05/Lincolnshire-CLEANING-DISINFECTION-AND-STERILIZATION-GUIDELINES-FOR-RE-USABLE-MEDICAL-DEVICES.pdf
[10] http://www.eurosurveillance.org. Case of legionnaires’ disease in a neonate following an home birth in a heated birthing pool. England, June 2014 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20857
[11] Water Regulations Advisory Scheme (WRAS). Fluid Categories. https://www.wras.co.uk/consumers/resources/glossary/fluid_categories/
[12] WHBN 00-10 Welsh Health Building Note. Part C: Sanitary assemblies2014, http://www.wales.nhs.uk/sites3/documents/254/WHBN%2000-10%20Part%20C.pdf
[13] Department of Health, Children, young people and maternity services. Health Building Note 09-02: Maternity care facilities, 2009.
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/147876/HBN_09-02_Final.pdf
[14] Freije, Matthew R. Some waterborne bacteria are tough, 2010. http://www.watertechonline.com/articles/some-waterborne-bacteria-are-tough
[15] Woolnough, Kevin. Legionella Expert Calls for Greater Vigilance, 2014. http://www.eurofins.co.uk/news-archive/legionella-expert-calls-for-greater-vigilance.aspx
[16] BEAMA. TMV Standards and regulations, 2013. http://www.beama.org.uk/en/product-areas/heating-hot-water–air-movement/thermostatic-mixing-valves/tmva-faqs-on-thermostatic-mixing-valves/tmv-standards-and-regulations.cfm
[17] Health and Safety Executive. Managing the risks from hot water and surfaces in health and social care, 2012. http://www.hse.gov.uk/pubns/hsis6.pdf
[18] Health and Safety Executive. Legionnaires’ disease The control of legionella bacteria in water systems, 2013. http://www.hse.gov.uk/pubns/priced/l8.pdf
[19] Health and Safety Executive. Managing legionella in hot and cold water systems. http://www.hse.gov.uk/healthservices/legionella.htm
[20] SMS Environmental – the water experts. Fluid Categories. http://www.sms-environmental.co.uk/fluid_categories.html.
[21] Nottingham University Hospitals NHS Trust. Legionella Management and Control Procedures, 2014.
Bibliography
- Ashford and St. Peter’s Hospitals, Women’s Health and Paediatrics Division (Abbey Birth Centre). Operational Policy and Clinical Guide, 2014.
- BASINGSTOKE AND NORTH HAMPSHIRE NHS FOUNDATION TRUST . CLEANING, DISINFECTION AND STERILISATION POLICY. Prod. Helen Campbell. BASINGSTOKE AND NORTH HAMPSHIRE, BASINGSTOKE AND NORTH HAMPSHIRE, 2010.
- BEAMA. TMV Standards and regulations. 2013. http://www.beama.org.uk/en/product-areas/heating-hot-water–air-movement/thermostatic-mixing-valves/tmva-faqs-on-thermostatic-mixing-valves/tmv-standards-and-regulations.cfm (accessed 2014 йил 24-09).
- Buckinghamshire Healthcare NHS Trust. Water birth and use of water in labour guideline. Prod. Miss G Tasker and Audrey Warren. 2013.
- Dekker, Rebecca. “Evidence on the Safety of Water Birth.” http://evidencebasedbirth.com/. 2014. http://evidencebasedbirth.com/waterbirth/ (accessed 2014 10-09).
- Department for Environment, Food and Rural Affairs. Water Supply (Water Fittings) Regulations 1999 Guidance Document relating to Schedule 1: Fluid Categories and Schedule 2: Requirements For Water Fittings. 1999. http://archive.defra.gov.uk/environment/quality/water/industry/wsregs99/documents/waterregs99-guidance.pdf.
- Department of Health. Children, young people and maternity services Health Building Note 09-02: Maternity care facilities. 2009.
—. “Health Building Note 00-09: Infection control in the built environment.” www.gov.uk. 2002. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/170705/HBN_00-09_infection_control.pdf (accessed 2014 6-12).
—. “Health Technical Memorandum 64: Sanitary assemblies.” 2006. http://www.wales.nhs.uk/sites3/documents/254/HTM%2064%203rded2006.pdf (accessed 2014 10).
—. “Water systems Health Technical Memorandum 04-01: Addendum” .2013. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/140105/Health_Technical_Memorandum_04-01_Addendum.pdf (accessed 01 2014-10).
—. “Water systems Health Technical Memorandum 04-01: The control of Legionella , hygiene, “safe” hot water, cold water and drinking water systems”. 2006.
- DH, Estates & facilities. Water systems Health Technical Memorandum 04-01: Addendum . Department of Health, Department of Health.
- Elizabeth R Cluett, Ethel Burns. Immersion in water in labour and birth. 2009.http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000111.pub3/abstract (accessed 2013 13-05).
- Elyse Fritschel, Kay Sanyal, Heidi Threadgill, and Diana Cervantes. Emerging Infectious Diseases.CDC. Centers for Disease Control and Prevention. CDC. 2014. http://wwwnc.cdc.gov/eid/article/21/1/14-0846_article (accessed 2015 5-January).
- Freije, Matthew R. Some waterborne bacteria are tough . 2010. http://www.watertechonline.com/articles/some-waterborne-bacteria-are-tough (accessed 2015 20-01).
- GOV.UK. Alert after Legionnaires’ disease case in baby. 2014. https://www.gov.uk/government/news/alert-after-legionnaires-disease-case-in-baby (accessed 2014 3-12).
- GOV.UK. Public Health England advice on home birthing pools. 2014. https://www.gov.uk/government/news/public-health-england-advice-on-home-birthing-pools (accessed 2014 03-August).
- Healio – Infectious Disease News. Legionellosis death after water birth sparks call for stricter infection control protocols. 2014. http://www.healio.com/infectious-disease/practice-management/news/online/%7Bfe352169-755d-4d21-9bb2-abb8ae209f89%7D/legionellosis-death-after-water-birth-sparks-call-for-stricter-infection-control-protocols (accessed 2015 07-01).
- Health and Safety Executive. Legionnaires’ disease The control of legionella bacteria in water systems. 2013. (accessed 2014 07-07).
—. “Legionnaires’ disease: Technical guidance.” 2013. http://www.hse.gov.uk/pubns/priced/hsg274part3.pdf (accessed 2014 20-10).
—. Managing legionella in hot and cold water systems. http://www.hse.gov.uk/healthservices/legionella.htm (accessed 2015 07-01).
—. “Managing the risks from hot water and surfaces in health and social care.” 2012. http://www.hse.gov.uk/pubns/hsis6.pdf (accessed 2014 20-11).
- Health Facilities Scotland. Consultation draft of SHTM 04-01 Water Safety for Healthcare Premises Part G: Operational Procedures and exemplar Written Scheme 2013. Health Facilities Scotland.
- Inquisitr. Oregon Water Birth Leaves Baby Disabled, Lawsuit Wants Labor Options Banned. 2015.http://www.inquisitr.com/1761136/oregon-water-birth-leaves-baby-disabled-lawsuits-wants-labor-options-banned/ (accessed 2015 16-01).
- Laura Franzin, Carlo Scolfaro, Daniela Cabodi, Mariangela Valera, and Pier Angelo Tovo. Legionella pneumophila Pneumonia in a Newborn after Water Birth: A New Mode of Transmission. Oxford Journals, November 2001: 104.
- Legionella Control. Birthing Pool Death Linked To Legionnaires disease. https://legionellacontrol.com/blog/166-birthing-pool-death-linked-to-legionnaires-disease (accessed 2014 27-11).
- Legislation.gov.uk. The Water Supply (Water Fittings) Regulations 1999.The National Archives. 1999. http://www.legislation.gov.uk/uksi/1999/1148/contents/made (accessed 2015 05-01).
- M.W. LeChevallier, World Health Organisation. Conditions favouring coliform and HPC bacterial growth in drinkingwater and on water contact surfaces . 2003.
- N Phin, T Cresswell, F Parry-Ford on behalf of the Incident Control Team. CASE OF LEGIONNAIRES’ DISEASE IN A NEONATE FOLLOWING A HOME BIRTH IN A HEATED BIRTHING POOL, ENGLAND, JUNE 2014.http://www.eurosurveillance.org. 2014. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20857 (accessed 2015 10-01).
- Nottingham University Hospitals. LEGIONELLA MANAGEMENT AND CONTROL PROCEDURES. May 8, 2014.
- Rosanna A. Zanetti-Daellenbach, Sibil Tschudin, Xiao Yan Zhong, Wolfgang Holzgreve, Olav Lapaire, Irene Ho ̈sli. Maternal and neonatal infections and obstetrical outcome in water birth . Prod. Women’s University Hospital Basel. Spitalstrasse, Basel: European Journal of Obstetrics & Gynecology and Reproductive Biology , 2006 28-August.
- SMS Environmental – the water experts. Fluid Categories. http://www.sms-environmental.co.uk/fluid_categories.html.
- Takuhito Nagai, Hisanori Sobajima, and Mitsuji Iwasa. A fatal newborn case of Legionella pneumophila pneumonia occurring after water birth in a bathtub with an all day circulating system, June 1999 – Nagoya City.http://idsc.nih.go.jp/. 2000. http://idsc.nih.go.jp/iasr/21/247/de2474.html (accessed 2014 17-06).
- Takuhito Nagai, Hisanori Sobajima, Mitsuji Iwasa, Toyonori Tsuzuki, Fumiaki Kura, Junko Amemura-Maekawa, and Haruo Watanabe. Neonatal Sudden Death Due to Legionella Pneumonia Associated with Water Birth in a Domestic Spa Bath. 2002.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC154682/ (accessed 2014 3-12).
- The Guardian. Legionnaires’ disease in baby is linked to heated birthing pool . 2014. http://www.theguardian.com/society/2014/jun/17/legionnaires-disease-heated-birthing-pool-baby-public-health (accessed 2014 18-June).
- U.S. Department of Health and Human Services Centers for Disease Control and Prevention (CDC) Atlanta, GA 30333. Guidelines for Environmental Infection Control in Health-Care Facilities . 2003.
- UNITED LINCOLNSHIRE HOSPITALS NHS TRUST. CLEANING, DISINFECTION AND STERILIZATION GUIDELINES FOR RE-USABLE MEDICAL DEVICES. Lincolnshire, 2010 January.
- Water Regulations Advisory Scheme. Fluid Categories . https://www.wras.co.uk/consumers/resources/glossary/fluid_categories/ (accessed 2014 3-12).
- which.co.uk. Having a water birth and using birth pools. http://www.which.co.uk/birth-choice/articles/using-water-in-labour.
- Woolnough, Kevin. Legionella Expert Calls for Greater Vigilance. http://www.eurofins.co.uk/news-archive/legionella-expert-calls-for-greater-vigilance.aspx (accessed 2015 17-01).
Please feel free to distribute and share this document crediting © K. D. Brainin (Active Birth Pools) 2015
The buoyancy of water helps mothers benefit from upright positions
Studies have shown that upright labour positions are associated with a reduced second stage, fewer episiotomies or instrumental intervention in contrast to mothers labouring on their backs.

Many women also feel empowered in an upright position, and experience a sense of control over their labour.
On land women need to contend with the force of gravity that limits their ability to assume upright postures especially as labour progresses and they feel tired.

Many women do not have the fitness or stamina to maintain upright postures for lengths of time.
The transition from the land to water helps revive and energise the mother giving her a new lease on life and sense of purpose.

The buoyancy of water supports the mother reducing her relative weight by approx. 33% (Archimedes Principle) allowing her to easily explore the full range of beneficial upright positions in comfort and move in ways that were not possible on land.

The space, depth and design features of Active Birth Pools allow women to move freely to find and be supported in the upright positions that are most comfortable and beneficial for a physiological labour to unfold.

The original models of our pools are still available
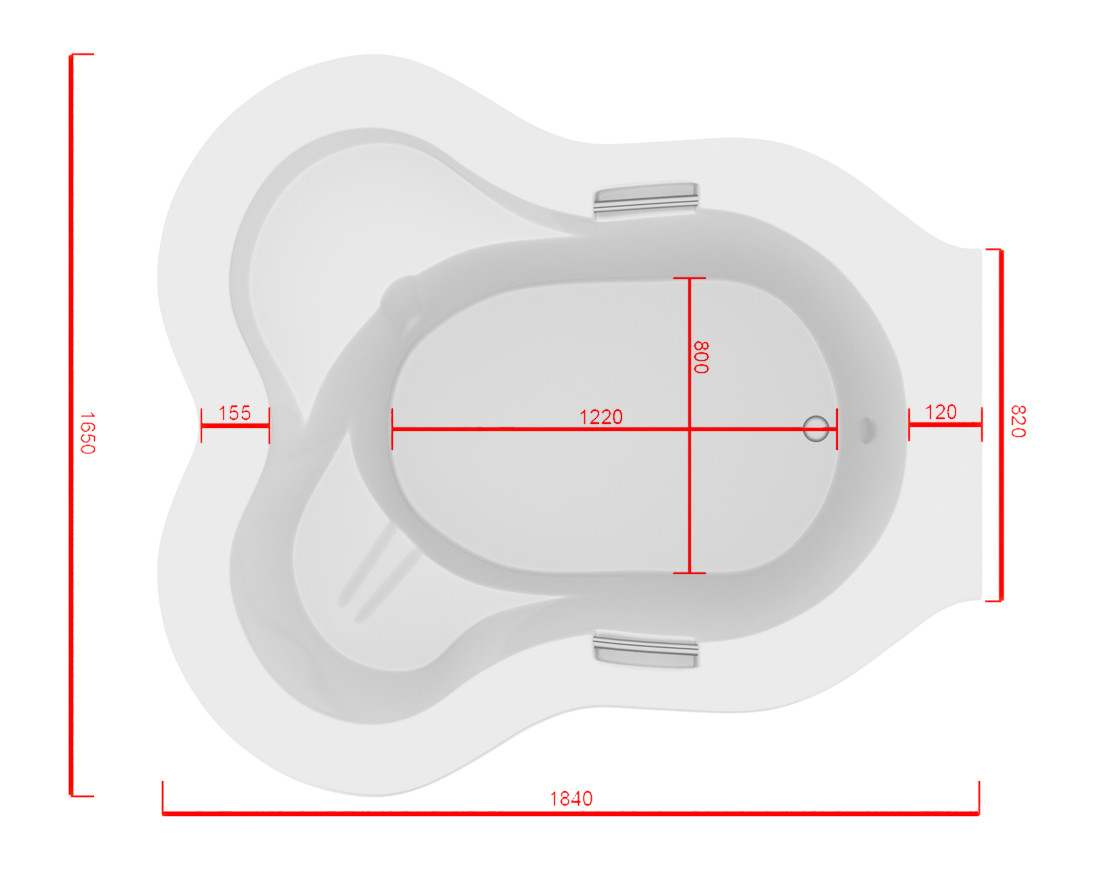
Active Birth Pool


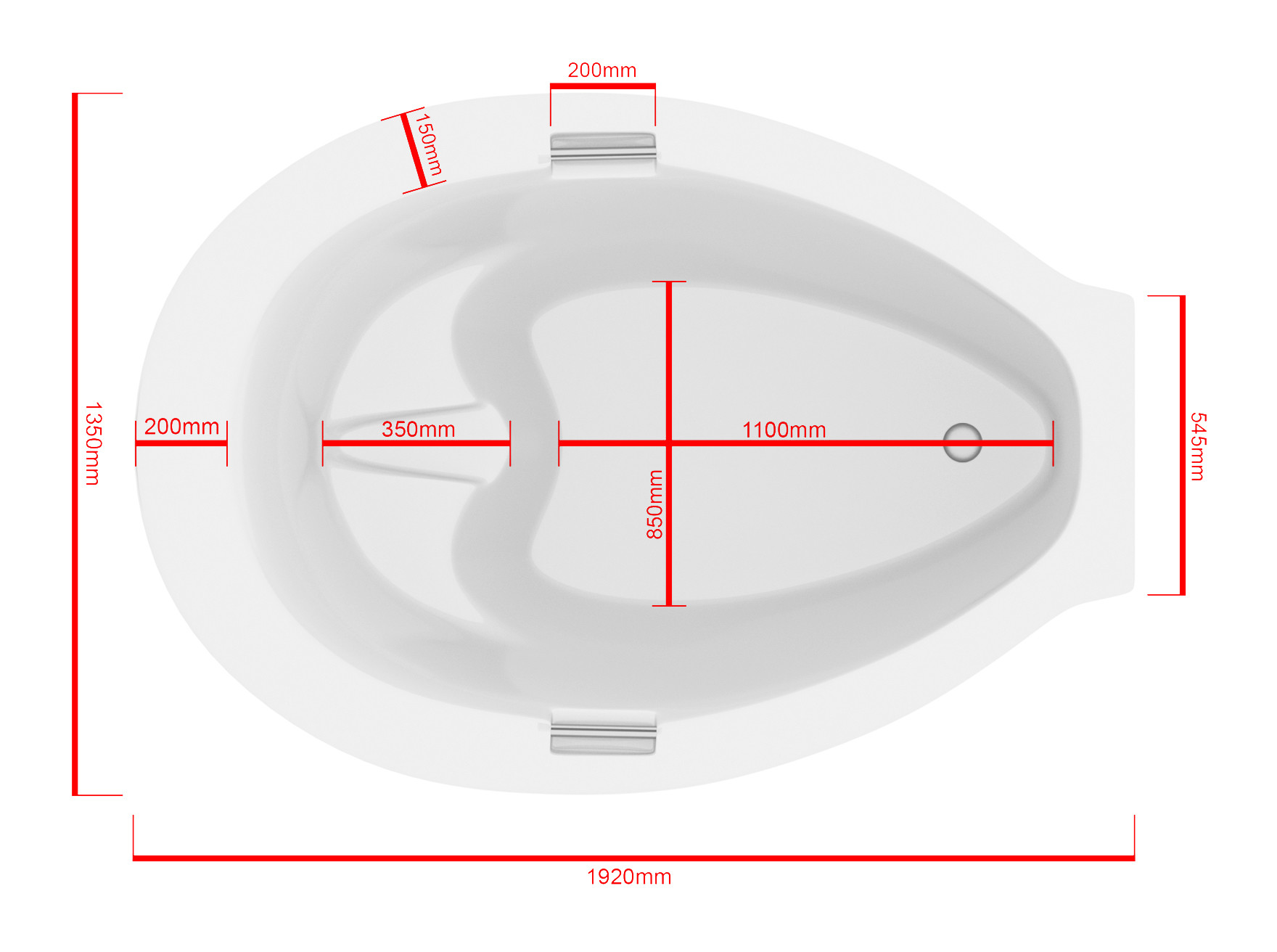
Venus Birth Pool


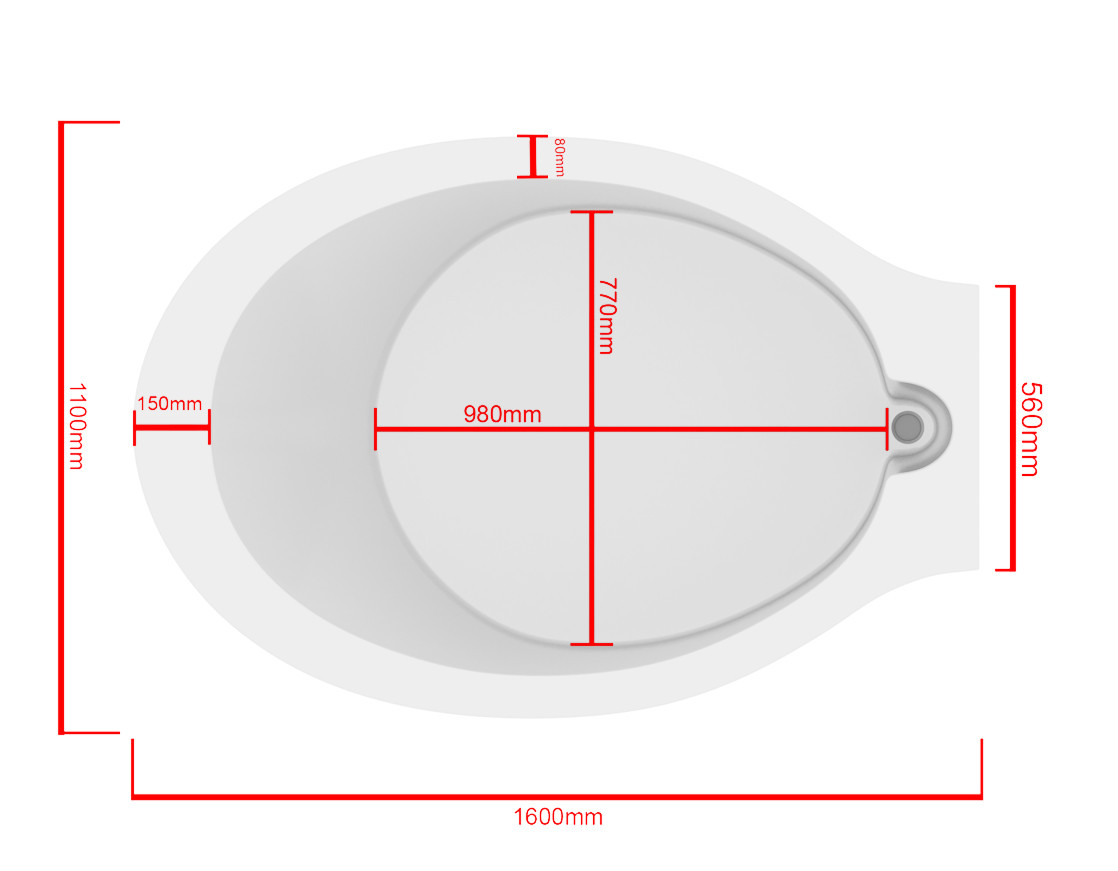
Princess Pool


These water birth pools are still available:
Why the Room You Give Birth In Should Be Like the Room You Conceived In
I remember first hearing of this concept from a talk that Michel Odent gave at the Active Birth Centre in London in the late 80’s.
It instinctively made sense to me.
Here’s why……
The concept of creating a birthing environment that mirrors the comfort and intimacy of the room where conception likely occurred holds significant merit.
Various studies and expert opinions emphasize the profound impact of the birthing environment on both the physiological and psychological aspects of childbirth.
The Impact of Environment on Physiological Birth
Research indicates that the environment in which a woman gives birth significantly influences the onset and progression of labor.
A calm, private, and safe ambiance is conducive to normal neuro-hormonal functioning, supporting the physiology of labor and birth.
This environment ideally should replicate the familiar, intimate setting akin to where conception might have occurred, as familiarity is linked to fewer medical interventions and greater maternal satisfaction.
Psychological Safety and Comfort
The psychological aspects of a birthing environment cannot be overstated.
Creating a home-like birth environment, similar to the personal and intimate setting of conception, significantly reduces the need for intrapartum analgesia and increases the likelihood of spontaneous vaginal birth and maternal satisfaction.
This is crucial, as the psychological state of the mother can profoundly impact the labor process.
The Role of Alternative Birth Settings
Alternative birth settings, such as bedroom-like rooms or ambient rooms, have been shown to increase the likelihood of spontaneous vaginal birth, breastfeeding at six to eight weeks, and women’s positive view of care.
These settings often include multi-sensory stimulations like vision, touch, sound, and aromas, which can be critical during labor and birth.
Creating a Supportive Environment
Elements like comfortable furniture, ability to control lighting and noise, and privacy are integral to creating a supportive birth environment.
These factors, reminiscent of a more personal and intimate setting, are crucial for ensuring a positive birthing experience.
The inclusion of familiar items and settings can play a pivotal role in mimicking the conception environment, thereby making the birthing process more natural and less stressful.
Conclusion
In essence, the room you give birth in should ideally reflect the room you conceived in due to its profound impact on the physiological and psychological aspects of childbirth.
Creating a familiar, comfortable, and intimate environment, similar to where conception occurred, can significantly enhance the birthing experience, leading to positive outcomes for both mother and child.
Enhancing Maternity Care: The Impact of the Birthing Environment and Water Birth Pools
The Economic and Patient-Centric Benefits of Water Birth Pools in Healthcare Facilities
The Warm Embrace: How Warm Water in Water Birth Pools Facilitates the Release of Oxytocin
Re-evaluating water birth temperature guidelines
Barbara Harper explores the effects of water temperature on mothers and babies.
Please click here to read the full article
Reasons to consider a water birth
Bridge to Health – Sian Smith
When considering their birth plan, more and more women are choosing to include the use of water at some stage.
In fact, around 30% of women now plan to use this method either for birthing their baby or as a natural way to reduce some of the intense sensations (pain!) associated with labour.
Here are some of the reasons why:

Water is relaxing!
Being able to bob around in a large pool of warm water is the perfect environment to help you stay calm and relaxed, in a situation most would normally consider pretty stressful.
For many, sliding into a warm bath is the ‘go to’ choice of relaxation after a hard day, so what better way to help you through one of the most physically demanding and memorable experiences of your life?
Additionally, a calmer birth may be less stressful for your baby, as moving from an environment of warm amniotic fluid to one of warm water is a gentle way of introducing them to their new surroundings.

Water is a natural pain reliever
The relaxing effects of water help encourage the body to produce its own pain-fighting substances.
This is beneficial both for Mum and baby; for Mum staying relaxed helps stimulate her natural production of oxytocin (the’ love hormone’ that helps the uterus contract) and endorphins, the ‘feelgood’ hormones that help work as a natural pain reliever.
For baby, a happy and relaxed Mum is more likely to birth quickly with a reduced need for medical intervention.

It reduces stress and anxiety
It is not just the water that helps to relax you. With a waterbirth, often the entire surroundings are altered to create a calming ambience e.g. dimmed lights and hushed voices.
This enables you to go into your own world much more easily than if in a harshly lit room with strange people popping in and out.
Additionally, this type of relaxation helps encourage deep abdominal breathing, preventing you from becoming tense which may make contractions feel more intense.

It reduces the risk of perineal tearing
The warmth of the water helps to promote increased blood flow to the vagina and perineum (the area between the vagina and anus that is susceptible to tearing during childbirth).
This increases flexibility of the tissues and can reduce the likelihood of tearing when birthing the baby’s head.

It allows you to adopt a more ‘active’ birth position
A reason that some women choose a water birth is that it allows you to retain some control throughout the labour process –being aware of the contractions and sensations your body is experiencing, with a reduced chance of medical intervention.
Additionally, the sensation of ‘weightlessness’ that being in the water provides, enables you to move around much more freely than your body has allowed you to for a while!
You are free to adopt almost any position that feels comfortable for you.
The classic image of a labouring woman is that of her laying on her back with her legs in stirrups.
Whilst this is the case for many, it is actually a fairly difficult way to birth your baby as you have to work against gravity to push the baby’s head UP and over the lowest part of the spine – the coccyx.
The best way to counteract this is to work with gravity and adopt a more ‘active’ squatting or modified squatting position.
Being in the water allows you to stay in these positions for longer, as you can lean against the side of the birthing pool for support.
Remaining fit, healthy and active will also help you have as smooth a pregnancy as possible.
Your Osteopath can advise you on exercises that are suitable throughout pregnancy, specifically core, pelvic and lower limb strengthening exercises that will help you be able to adopt active birth positions and use the correct muscles to birth your baby as efficiently as possible.

It is safe!
Of course, water births are not suitable for everyone – the main criteria is that Mum and baby must be healthy, the baby must be in a head-down position, and the pregnancy must be between 37 and 42 weeks.
But as the majority of pregnancies are healthy, a water birth can offer a natural and more in control option to the labour choices a woman has.
And finally, one of the most frequently asked questions regarding waterbirths appears to be ‘will my baby drown underwater?’… to which the answer is no!
The baby receives all of its oxygen via the placenta and hormones circulating through the baby ensure this occurs until the baby is lifted out of the water.
It is also known as the ‘foetal dive reflex’ and allows babies to be underwater for short periods of time up until around 6 months old.
The benefits of labouring in water for overweight and obese mothers
Excerpt from article published by Big Birtha who provides information and support for bigger mums and mums to be.
All women are more buoyant and supported by water, it’s one of the reasons swimming and aqua aerobics are particularly good forms of exercise while pregnant.
But the benefit is likely to be greater for obese women, as fatter bodies are naturally more buoyant.
The buoyancy and support provided by water eases movement, which may make both maintaining an active labour and facilitating access for monitoring easier.
On land, it is cumbersome and difficult for a heavily pregnant woman of any size to quickly move between kneeling, reclining, sitting, leaning, crouching, turning from front to back etc.
In water, it is simple and easy to shift to whatever position is most comfortable/convenient, even midway through contractions.
Being in water also promotes positions which are more agreeable for birthing. Lying flat on your back on a bed is one of the worst positions to be in during labour.
When you are on your back you are working against gravity; actually trying to push the baby out uphill.
It’s only a slight incline, but it’s there.
To add to the problem, when lying down, your body weight is also resting on your coccyx (tailbone), forcing it into the pelvic cavity and reducing space for the baby.
In water, even if you were to float on your back, you wouldn’t be putting the same pressure on your tailbone, and you are far more likely to take an upright position, crouching or kneeling, for instance; positions which on land are uncomfortable to maintain, but not in water.
This frees up your coccyx to keep out of the way.
It is well documented that warm water reduces pain felt by labouring women, and decreases the use of other pain relief.
Given the issues with providing epidural anaesthesia to obese women, it seems sensible that using water; an effective non-pharmaceutical intervention to help with pain should be an attractive alternative?
Obese women are at increased risk of having longer labours, and of moving on to instrumental delivery and caesarean sections for ‘failure to progress’.
Yet immersion in water has been shown to significantly reduce the length of labour in ‘normal’ sized women.
It doesn’t take much of a leap of imagination to consider that water might help to address this problem, at least in some obese women?
Active Birth Pools are specially designed for to accomodate bigger mothers enabling them to move and benefit from the positions natural to labour and birth.
Various means of entry and exit from the pool as well as emergency evacuation have been considered and designed for to safeguard over weight mothers and the midwives who care for them.
Groundbreaking research confirms benefits of water birth
Systematic review and meta-analysis to examine intrapartum interventions, and maternal and neonatal outcomes following immersion in water during labour and waterbirth
Library of Medicine
Abstract
Objectives: Water immersion during labour using a birth pool to achieve relaxation and pain relief during the first and possibly part of the second stage of labour is an increasingly popular care option in several countries. It is used particularly by healthy women who experience a straightforward pregnancy, labour spontaneously at term gestation and plan to give birth in a midwifery led care setting. More women are also choosing to give birth in water. There is debate about the safety of intrapartum water immersion, particularly waterbirth. We synthesised the evidence that compared the effect of water immersion during labour or waterbirth on intrapartum interventions and outcomes to standard care with no water immersion. A secondary objective was to synthesise data relating to clinical care practices and birth settings that women experience who immerse in water and women who do not.
Design: Systematic review and meta-analysis.
Data sources: A search was conducted using CINAHL, Medline, Embase, BioMed Central and PsycINFO during March 2020 and was replicated in May 2021.
Eligibility criteria for selecting studies: Primary quantitative studies published in 2000 or later, examining maternal or neonatal interventions and outcomes using the birthing pool for labour and/or birth.
Data extraction and synthesis: Full-text screening was undertaken independently against inclusion/exclusion criteria in two pairs. Risk of bias assessment included review of seven domains based on the Robbins-I Risk of Bias Tool. All outcomes were summarised using an OR and 95% CI. All calculations were conducted in Comprehensive Meta-Analysis V.3, using the inverse variance method. Results of individual studies were converted to log OR and SE for synthesis. Fixed effects models were used when I2 was less than 50%, otherwise random effects models were used. The fail-safe N estimates were calculated to determine the number of studies necessary to change the estimates. Begg’s test and Egger’s regression risk assessed risk of bias across studies. Trim-and-fill analysis was used to estimate the magnitude of effect of the bias. Meta-regression was completed when at least 10 studies provided data for an outcome.
Results: We included 36 studies in the review, (N=157 546 participants). Thirty-one studies were conducted in an obstetric unit setting (n=70 393), four studies were conducted in midwife led settings (n=61 385) and one study was a mixed setting (OU and homebirth) (n=25 768). Midwife led settings included planned home and freestanding midwifery unit (k=1), alongside midwifery units (k=1), planned homebirth (k=1), a freestanding midwifery unit and an alongside midwifery unit (k=1) and an alongside midwifery unit (k=1). For water immersion, 25 studies involved women who planned to have/had a waterbirth (n=151 742), seven involved water immersion for labour only (1901), three studies reported on water immersion during labour and waterbirth (n=3688) and one study was unclear about the timing of water immersion (n=215).Water immersion significantly reduced use of epidural (k=7, n=10 993; OR 0.17 95% CI 0.05 to 0.56), injected opioids (k=8, n=27 391; OR 0.22 95% CI 0.13 to 0.38), episiotomy (k=15, n=36 558; OR 0.16; 95% CI 0.10 to 0.27), maternal pain (k=8, n=1200; OR 0.24 95% CI 0.12 to 0.51) and postpartum haemorrhage (k=15, n=63 891; OR 0.69 95% CI 0.51 to 0.95). There was an increase in maternal satisfaction (k=6, n=4144; OR 1.95 95% CI 1.28 to 2.96) and odds of an intact perineum (k=17, n=59 070; OR 1.48; 95% CI 1.21 to 1.79) with water immersion. Waterbirth was associated with increased odds of cord avulsion (OR 1.94 95% CI 1.30 to 2.88), although the absolute risk remained low (4.3 per 1000 vs 1.3 per 1000). There were no differences in any other identified neonatal outcomes.
Conclusions: This review endorses previous reviews showing clear benefits resulting from intrapartum water immersion for healthy women and their newborns. While most included studies were conducted in obstetric units, to enable the identification of best practice regarding water immersion, future birthing pool research should integrate factors that are known to influence intrapartum interventions and outcomes. These include maternal parity, the care model, care practices and birth setting.
Prospero registration number: CRD42019147001.
Keywords: Maternal medicine; PRIMARY CARE; Pain management.
Research review backs benefits of water births for mothers and babies
Nursing Times
Water births provide “clear benefits” over standard care for healthy mothers and their newborns, according to UK researchers.
They found water births were associated with fewer interventions and complications during and after the birth, as well as higher levels of satisfaction for the mother.
“Water immersion is an effective method to reduce pain in labour, without increasing risk”
Study authors
Researchers compared the extent of healthcare interventions needed during and after labour to see if outcomes differed between a water birth and standard care – without a birthing pool.
They noted that a water birth involves using a birthing pool to achieve relaxation and pain relief, with the mother either exiting the pool for the birth, so the newborn can emerge into air to breathe, or remaining in the pool and bringing the newborn to the surface to start breathing.
They trawled research databases looking for relevant studies published over 20 years between 2000 and 2021, finding 36 studies involving 157,546 women. Most were carried out in obstetric units.
The study results showed that a water birth, regardless of whether women birth in or out of the pool, “has clear benefits to women” in obstetric units, where most births take place and where interventions and complications are more likely than in midwife-led units.
A waterbirth was as safe as standard care for healthy mothers and their newborns, they said in the journal BMJ Open.
Compared with standard care, a water birth significantly reduced the use of epidurals, injected opioids, episiotomy, as well as pain and heavy bleeding after the birth.
In addition, it increased mothers’ satisfaction levels and the odds of an intact perineum. There was no difference in the rate of Caesarean sections, said the study authors from Oxford Brookes University.
“Water immersion can significantly increase the likelihood of an intact perineum and reduce episiotomy, an intervention which offers no perineal or foetal benefit, can increase postnatal pain, anxiety, and impact negatively on a woman’s birth experience,” they said.
However, they observed more instances of umbilical cord breakage among water births, but the rate was still low – 4.3 per 1,000 births in water compared with 1.3 per 1,000 births with standard care.
This finding may be linked to pulling on the umbilical cord when the newborn is brought up out of the water, the researchers suggested.
Overall, they stated: “Water immersion provides benefits for the mother and newborn when used in the obstetric setting, making water immersion a low-tech intervention for improving quality and satisfaction with care.
“In addition, water immersion during labour and waterbirth alter clinical practice, resulting in less augmentation, episiotomy, and requirements for pharmacological analgesia,” they said.
They concluded: “Water immersion is an effective method to reduce pain in labour, without increasing risk.”
However, they acknowledged that information on birth settings, care practices, interventions and outcomes varied considerably among the included studies, and few were carried out in midwife-led units or in the mother’s home, which may have affected the findings of the analysis.
To strengthen the evidence base, future research should include factors that are known to influence interventions and outcomes during and after labour or birth, they added.
For example, how many children a woman has already had, where she gives birth, who looks after her, and the care she receives.
“The challenge now is to ensure this choice is open to all women wherever they live”
Clare Livingstone
Commenting on the research, Clare Livingstone, professional policy advisor at the Royal College of Midwives, said: “This is really good news for women choosing to have a water birth or thinking of having one.
“There has been previous research outlining the benefits for women and this significant study adds weight to those. It is also positive because it is more information for women when deciding how they want to give birth.”
She said: “Water births are becoming more widely available for women across the UK, but this isn’t the case everywhere. The challenge now is to ensure this choice is open to all women wherever they live.”
Ms Livingstone added: “What is needed now is to see more research into water births in midwife-led settings and in women’s homes. This will give us a broader picture of the impact of water births.”
Birth under water – Michel Odent
Michel Odent’s groundbreaking report “Birth Under Water” that was published in the Lancet in December 1983 is widely regarded as the seminal moment in time when the use of water for labour and birth entered our consciousness.
I’d personally like to thank Michel for being the inspiration that led me to begin to create and develop water birth pools in 1987 and for facilitating the birth of my son Theo at home in 1988.
Keith Brainin – Founder & Director Active Birth Pools

Birth under water – Michel Odent
Originally published in the Lancet: 1983
Centre Hospitalier Général de Pithiviers, PIthiviers 45300, France
The 100th birth under water in our hospital in June provided my team with an opportunity to summarise our experience of the use of water in an obstetric unit.
Since a report on birth under water in 1805,1 the subject has been rarely broached in the medical literature.
In Pithiviers, a hospital which is, in other respects, a conventional state hospital,2 a small pool has been installed close to the homely birthing room.
This pool is large enough (2m in diameter) and deep enough (about 0.7m) to make it easy for a woman in it to change her posture.
Many parturients feel and irresistible attraction to water. We don’t advise women to try the pool; we simply offer the pool as a possibility.
The water is ordinary mains tap water, at a temperature of 37 °C. The water is not sterilized, and contains no chemicals or additives on any sort.
We tend to reserve the pool for women who are experiencing especially painful contractions (lumbar pains, in particular), and where the dilation of the cervix is not progressing beyond about 5cm. In these circumstances, there is commonly a strong demand for drugs.
In most cases, the cervix becomes fully dilated within 1 or 2 hours of immersion in the pool, especially if the lights are dimmed.
It is possible to check the fetal heartbeat regularly with a small ultrasound stethoscope or with a traditional obstetrical stethoscope. Most women choose to leave the water in the second stage.
We believe that the warm pool facilitates the first stage of labour because of the reduction of the secretion of nor-adrenaline and other catecholamines; the reduction of sensory stimulation when the ears are under water; the reduction of the effects of gravity; the alteration of nervous conduction; the direct muscular stretching action; and peripheral vascular action.
Other factors, however, are difficult to rationalise. We have found, for example, that the mere sight of water and the sound of it filling the pool are sometimes sufficient stimuli to release inhibitions so that a birth may occur before the pool is full.
We have observed that water seems to help many parturients reach a certain state of consciousness where they become indifferent to what is going on around them.
Although nearly all the women who enter the pool leave it before birth, the process of delivery can sometimes be so extraordinarily fast under water, that some parturients do not leave the pool at the second stage.
Birth under water is therefore not exceptional in our unit, although it may not be intentional. During the second stage, immersion in warm water seems to help women to lose inhibitions. Most women cry out freely during the last contractions.
When the birth happens under water, the newborn infant is brought gently to the surface and placed in the mother’s arms. This is always done within seconds but without rushing (I am present at the pool for every underwater delivery).
Our experience confirms that the newborn’s first breathing is triggered by contact with the air and the sudden difference in temperature.
There is no risk of inhalation of water. It is useful to remember that in the human species carotid chemoreceptors are thought to be insensitive at birth, and very likely play no part at the time of the first cry. 3,4,5 Only 2 newborn infants out of 100 needed suction of the upper respiratory tract and a short period of manual ventilatory support.
At the time of first contact, most mothers are in a vertical position, kneeling in the water. They hold the baby in their arms in such a way that skin-to-skin and eye-to-eye contact are as perfect as possible.
An early demonstration of the rooting reflex is almost the rule, and a first sucking 20 min after the birth is common.
Water seems to facilitate the development of the mother-infant relationship. We cut the umbilical cord and help the mother leave the pool just before expulsion of the placenta.
We consider that there might be a risk of water embolism if the mother were to stay in the pool after this time. In 100 underwater deliveries there were 2 manual removals of placenta (our general rate is less than 1%).
All the presentations were cephalic. In breech presentations, our strategy is to use the first stage as a test before deciding on either a vaginal delivery or a caesarian section: in these cases we prefer not to interfere with drugs or with a bath.
Among the 100 women who gave birth underwater, there were 43 primipara, 37 secundiparas, 14 para 3, 2 para 4, one para 5, one para 6, and one para 7.
The youngest was 19 and the oldest was 43. The average age was 28. The lowest birth weight was 2.15kg and the highest was 4.40 kg, we did not perform any episiotomies.
All the tears (of which there were 29) were first degree. We had no infectious complications, even where the membranes were already broken.
There were no perinatal deaths. One infant was transferred to a paediatric unit one day after the birth with groaning and respiratory failure, symptoms which were diagnosed as subarachnoid haemorrhage after delivery in the posterior position at 37 weeks.
Only one infant was jaundiced and required phototherapy (15mg/dl bilirubin on the second day). One of the infants born under water died suddenly some weeks later, although it was previously considered to be perfectly healthy.
We have found no risk attached either to labour or to birth under water, and in any hospital where a pool is in daily use, a birth under water is bound to happen now and then.
Compared with the supported squatting position in the birthing room, we have found that the end of the second stage of labour can be more difficult under water, particularly for primipara, but immersion during the second half of the first stage of labour is helpful, particularly for parturients having painful and insufficient contractions.
It should be possible for any conventional hospital to have a pool situated close to the birthing room and operating theatre.
The use of warm water during labour requires further research, but we hope that other experience would confirm that immersion in warm water is an efficient, easy, and economical way to reduce the use of drugs and the rate of intervention in parturition.

REFERENCES
1. Embry M. Observation sur un accouchement terminé dans le bain. Ann Soc Méd Prat Montpellier 1805; 5: 13.
2. Gillett J. Chilbirth in Pithiviers, France. Lancet 1979; ii: 894-96.
3. Girard F, Lacaisse A, Dejours P. Lestimulus O 2 ventilatoire à la période néonatale chez l’homme. J Physiol (Paris) 1960; 52: 108-09.
4. Purves MJ. The effects of hypoxia in the newborn lamb before and after denervation of the carotid chemoreceptors. J Physiol 1966; 185: 60-77.
5. Purves MJ. Chemoreceptors and their reflexes with special reference to the fetus and newborn. J Devl Physiol 1981; 3: 21-57.
Ventilation for the birthing environment
Engineering experts Phil Nedin and Dr. Anna Coppel from Arup’s advanced Technology and Research team look at the science of ventilating a birthing room.
Water Birth Pools expel a high volume of moisture that must be considered when designing the ventilation system for a water birth room.
Ventilation for birthing pool facilities

Sheila Kitzinger – Birth in Water: Just a Fad?
Originally published December 11, 2014
World-renowned social anthropologist and birth activist Sheila Kitzinger (1929-2015) was a strong advocate for birth in water, known as waterbirth.
A voice for the ability for every woman to choose, Sheila believed that waterbirth should be an option in mainstream maternity care.

In this piece for Birth Institute, Sheila outlined some of the myths surrounding the birth method, and provides evidence that, in fact, waterbirth is a safe, effective and empowering birthing option.
Learn how to support women through labor and delivery in water. Become a midwife!
Waterbirth is often discussed as if it were a novelty – and a dangerous one at that. It has been assumed to be something that “dropouts” and “weirdoes” choose, or that it is just a recent, passing phenomenon.
In truth, birthing in water is a safe and widespread practice among hospitals in the UK and Western Europe – including Switzerland, Italy, Spain, Portugal, Malta, Denmark, Norway and Finland.
Furthermore, most practices aren’t as new as we think (the Ostend Aquanatal Centre in Belgium has been going strong since the late 80s), and waterbirth practices are here to stay.
Birth in water is safe and effective
Swiss study reveals that when using a pool women require less analgesia, have a lower incidence of perineal trauma, and reduced blood loss at delivery.
NICE (National Institute for Health and Care Excellence) concludes that waterbirth ‘provides the safest form of pain relief’.
There is evidence that being in water improves uterine contractility and speeds dilatation. So, awoman giving birth in water is less exposed to interventions, including artificial augmentation of uterine activity, and is more likely to feel happy about her birth experience afterwards.
Yet that may not only be due to the water. Labouring women who give birth in water have more one-to-one care from a midwife they have come to know.
This, combined with a relaxed environment in which the pool is used, contributes to the positive results. More first time mothers have spontaneous births in a freestanding midwifery center or at home than those in hospital.
In the UK, the NHS (National Health Service) states that women should be able to use a pool if they wish, and recommends one be available for every thousand women.
This option has become part of mainstream maternity care, and approximately 75% of all hospitals in the UK have installed birthing tubs.
Many community midwives are eager to raise the homebirth rate, and portable pools, designed to be used by just one woman (to avoid cross-infection), are selling well.
Complicated waterbirthing pools are not necessary.
Chairs, stools and other contraptions restrict movement, and when a woman is immobilized she is more likely to need obstetric intervention.
Francoise Freedman of Birthlight in Cambridge suggests using a pool at home to explore yoga movements during pregnancy.
These include hip-openers, kneeling stretches, and those to prevent and ease back pain, and others for ribcage expansion and pelvic floor toning.
The warm water acting as a cushion also makes a comfortable space to practice perineal massage.
Waterbirth is here to stay
Midwives keen on home birth and waterbirth were once seen as dissidents and mavericks.
This has changed now – so much that in the UK, it is common to encourage women to choose to labour, and perhaps give birth, in water and in their own home. Pregnant women and midwives are being empowered now.
Every midwife-run and staffed birth center for low risk women offers pools, and midwives are beginning to develop the skills to use them. There is a feast of research from which midwives can learn more.
Ethel Burns, Waterbirth Practitioner, Research Midwife and Midwifery Teacher, and I have drawn up recommendations for practice in a paper available from Oxford Brookes University (read it here).
Sheila Kitzinger (1929-2015) was a social anthropologist of birth and an advocate of home births. She believed that women have the right to decide the place of birth and kind of care they prefer, and to make an informed choice, based on research and their own values.
Women suffering post-traumatic stress after birth would ring her for help, seeking the confidence to deal with it. For years she worked with mothers and babies in prison and asylum centers. She lectured all over the world and her books are published in 23 languages.
Exploring movements in Water
Sheila was a keen proponent of water birth.
Her wonderful article gives us examples of the type and range of movements natural to labour and birth that mothers explore in water.
The pool in the photos is an original Oval Portable Water Birth Pool circa 1987 – to my knowledge the first specially designed portable water birth pool ever produced.
Please click here for a copy of Exploring movements in water:
How to restore your old birth pool to pristine condition
We’ve been supplying water birth pools to hospitals since 1989.
Many of the pools we supplied in the 90’s are still in active service!
Below Venus Pool at the Royal Berkshire Hospital 1992 – still in use today

We occasionally receive reports that the pools are not looking as clean and bright as they originally were.
Not to worry.
There is a product called tide mark cleaner that was developed for spas and swimming pools.
You can either use it to remove stains or brighten up the appearance of the pool when necessary.
It will restore your pool to pristine condition.
Here’s a link:
http://www.amazon.co.uk/Waterline-Cleaning-removes-lines-cleaner/dp/B006DFD7VK
For information about cleaning and disinfection procedures please click here.
Water Birth Pools: The economic reality and impact
I wrote this article a few years ago.
It seems particularly relevant now.

Recent news has highlighted the restrictive financial environment that maternity units will be expected to operate in.
Yet, at the same time midwives are charged with the important task of improving the quality of care and services.
David Cameron has said, “The whole aim of these NHS reforms is to make sure we get the value for the money we put in.”[1]
In the same article, Stephen Dorrell, former Health Secretary commented that, “In real terms, the NHS budget was being broadly maintained, but we’re having to find ways of doing more with the same amount of money.”[2]
The only way of improving maternity services is by optimising facilities, saving money wherever practical and normalising childbirth to a far greater extent.

Studies have shown that women who are supported during labour need to have fewer painkillers, experience fewer interventions and give birth to stronger babies.
After their babies are born, supported women feel better about themselves, their labour and their babies.
A focus on normalising birth results in better quality, safer care for mothers and their babies with an improved experience.
Increasing normal births is associated with shorter (or no) hospital stays, fewer adverse incidents and admissions to neonatal units and better health outcomes for mothers.

It is also associated with higher rates of successful breastfeeding and a more positive birth experience.
These changes benefit not only women and their families but also maternity staff. Midwives are able to spend less time on non-clinical tasks and more on caring for women and their babies.
Psychologically speaking, and in particular for first time mothers, the less intervention and a more hands on approach with one-to-one support means that mothers will leave hospital feeling held and therefore far better prepared for motherhood.
This again has a domino effect, not just on the welfare of the infant, but also circumventing the need for costly government and LA interventionist approaches in particular for younger mothers post-partum.

What increases the likelihood of normal births?
It is also known that some factors help to facilitate straightforward birth without evidence of additional risks, including one-to-one support, immersion in water for low-risk women, planning for a home birth, care from known midwives, more extensive training of junior doctors, employment of consultant midwives focusing on normality, and support on the labour ward from consultant obstetricians[3].
How can midwives make a case for purchasing birth pools?
The need for more water birth facilities is evident. The problem is that financial controllers are under pressure to save money.
They will not be easily convinced of the necessity unless you clearly stress that purchasing pools should not be viewed as a cost but rather to make the case that they are a valuable investment and will enable your unit to optimise resources, improve the quality of care and yield a return of significant financial savings.
A birth pool is a simple, inexpensive piece of medical equipment that can have a major impact on the quality of care and cost of having a baby.
The bed is no longer the primary focus of the room: having birth pools in hospitals and delivery suites facilitates pain relief encourages relaxation and therefore confidence and promotes mobility along with soft furnishings such as beanbags.

Importantly, this results in significant financial savings!
Our cost study has revealed that savings of up to £700.00 per birth can be achieved.
For example, St Richards Hospital in Chichester has three of our birth pools as well as our soft furnishings.
They recently reported their first successful VBAC in the pool for a woman who had previously had twins by c-section.
Depending on complications, a c-section costs between £1,370 and £1,879 in contrast to a normal delivery that is usually between £735 and £1,097.[4]
The experience of hospitals that have birth pools demonstrates that the cost of installing a pool is soon recouped by the savings achieved through reduced use of medical methods of pain relief and shorter hospital stays.
Wherever possible, women should have the opportunity to labour in water, as this is often far more comfortable.
The NHS has advised hospitals to ensure facilities are in place for this: three pools for 1,000 births a year is seen as adequate provision[5].
[1] BBC: 19/01/11
[2] BBC 19/01/11 taken from BBC Radio 4 Today programme
[3] Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD003766. DOI: 10.1002/14651858.CD003766.pub2
[4] NHS Institute, 2009
[5] NHS Guidelines on Childbirth 26 September 2007
The case for the wide-spread development of water birth facilities
In light of the publication of recent articles that report the growing demand from women around the world who want to have a natural, drug free, non-medicalised birth (Weiss 2014 and Gilbert 2015) we need to look at ways to help them have this experience.
If they are not going be reliant on analgesia for pain relief they need options to help them cope with the pain to allow a physiological labor to unfold.
Immersion in warm water has been unequivocally proven to be of great benefit both physiologically and psychologically.
It is not important if the baby is born in water.
In fact, water birth should be de-emphasised as it is a controversial issue in many parts of the world.
The key point and main benefit that needs to be made and focused on is how women who enter a warm pool of water in established labour with strong contractions find that they are able to cope with the pain and have a natural birth.
Women have a greater sense of fulfillment and accomplishment and babies experience a non-traumatic birth.
Aside from the obvious benefits to mothers and babies, midwives experience greater job satisfaction and hospitals save money and optimise resources from the reduced use of analgesia, medical intervention and shorter hospital stays.
Nearly a third of women benefited from the use of a water birth pool in the UK in 2014 (National Maternity Survey 2014).
With up to 60% of mothers open to natural birth now is the time for midwives, obstetricians and hospitals to consider making this safe, low cost option available.
Studies have shown that upright labour positions are associated with a reduced second stage, fewer episiotomies or instrumental intervention in contrast to mothers labouring on their backs. (Gupta, Hofmeyr and Shehmar 2012 and Gupta and Nikodem 2000).
Many women also feel empowered in an upright position, and experience a sense of control over their labour (Balaskas 2001).
On land women need to contend with the force of gravity that limits their ability to assume upright postures especially as labour progresses and they feel tired.
Many women do not have the fitness or stamina to maintain upright postures for lengths of time. (Gupta JK, Hofmeyr GJ, Smyth R 2007).
The transition from the land to water helps revive and energise the mother giving her a new lease on life and sense of purpose.
The buoyancy of water supports the mother reducing her relative weight by approx. 33% (Archimedes Principle) allowing her to easily explore the full range of beneficial upright positions in comfort and move in ways that were not possible on land.
The calming, relaxing effect of the warm water promotes the flow of oxytocin, a powerful hormone that plays a huge role in childbirth, causing the uterus to contract and triggering the ‘fetal ejection reflex’.
Michel Odent has expounded upon the beneficial physiological effect that immersion in water during labour has on hormone secretion, including observations that women entering warm water experience oxytocin surges which can advance dilation and stimulate contractions (Odent 2014).
The economic impact
Studies have shown that women who are supported during labour need to have fewer painkillers, experience fewer interventions and give birth to stronger babies.
A focus on normalising birth results in better quality, safer care for mothers and their babies with an improved experience.
Increasing normal births is associated with shorter (or no) hospital stays, fewer adverse incidents and admissions to neonatal unit and better health outcomes for mothers.
It is also associated with higher rates of successful breastfeeding and a more positive birth experience.
These changes benefit not only women and their families but also maternity staff.
Midwives are able to spend less time on non-clinical tasks and more on caring for women and their babies.
Psychologically speaking, and in particular for first time mothers, the less intervention and a more hands on approach with one-to-one support means that mothers will leave hospital feeling held and therefore far better prepared for motherhood.
This again has a domino effect, not just on the welfare of the infant, but also circumventing the need for costly government and interventionist approaches in particular for younger mothers post-partum.

The experience of hospitals that have birth pools demonstrates the savings achieved through reduced use of medical methods of pain relief and shorter hospital stays.
Setting up a water birth facility
Hospitals in the United Kingdom have been evolving clinical guidelines for the use of water for labour and birth for over 3o years.
The protocols for operational policy that they’ve developed are widely regarded as the benchmark standard internationally.
Below a collection of guidelines and publications to help you create a water birth facility.
Clinical Guidelines – Royal Cornwall Hospital
Clinical Guidelines – Royal Worcester Hospital
Guideline for the Management of Women Requesting Immersion in Water – Norfolk and Norwich University Hospitals
Operational Policy and Clinical Guidelines – Abbey Birth Centre
Birthspace: An evidence-based guide to birth environment design – Queensland Centre for Mothers and Babies
Use of water for labour and birth – Hywel DDA Local health Board
Guidelines for use of pool during labour and delivery – East Cheshire NHS Trust
Guiding principles for midwifery care during normal labour – Barking, Havering and Redbridge NHS Trust
Waterbirth care during labour for low risk women – Sandwell and West Birmingham Hospitals
Waterbirth Guidelines – Midwifery Led Unit, Wirral Hospital
Choosing a Water Birth – East and North Hertfordshire
Birthing pool use of labour and delivery – Wansbeck General Hospital
Water birth and use of water in labour guideline – Buckinghamshire Healthcare
Water for labour and birth guideline – Northern health and Social Care Trust
Immersion in water during labour and birth – NHS Forth Valley
Intrapartum care midwifery led unit – Wirral Women & Children’s Hospital
Guidelines for water birth within the hospital and at home – Dartford & Gravesham NHS
Disinfection and Sterilisation policy (infection control) – Basingstoke and North Hampshire NHS FT
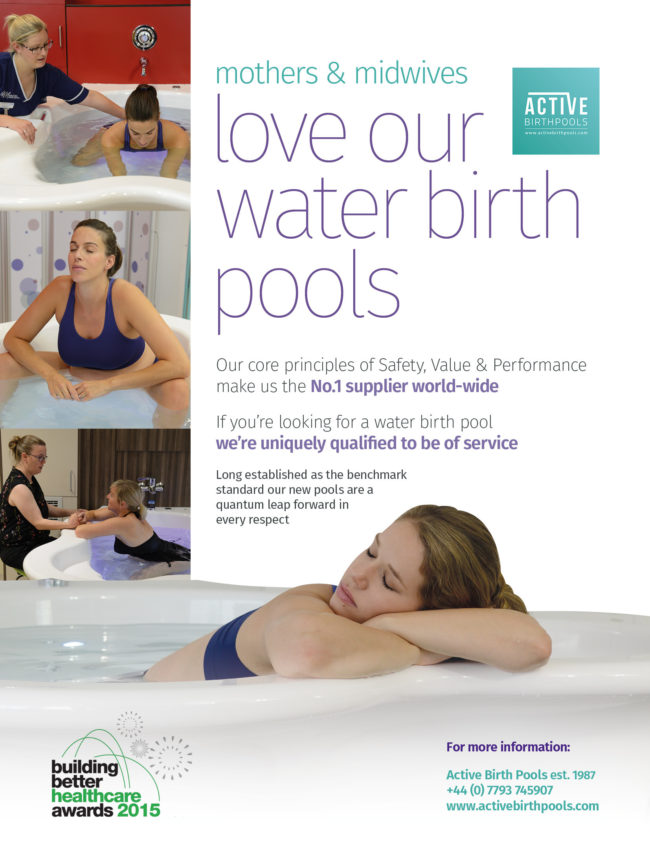
Nothing helps mothers cope with pain in labour more effectively
Water birth pools play a vital role in helping mothers experience physiological labour and natural birth.
Nothing helps mothers cope with pain more effectively.

If mothers are not going be reliant on analgesia for pain relief they need other options.
Mothers who enter a pool of warm water in established labour find that they are better able to cope with the pain.
Immersion in warm water has been unequivocally proven to be of great benefit both physiologically and psychologically.

Women have a greater sense of fulfillment and accomplishment and babies experience a non-traumatic birth.
Aside from the obvious benefits to mothers and babies, midwives experience greater job satisfaction and hospitals save money & optimise resources.
Nearly a third of women benefited from the use of a water birth pool in the UK in 2014 (National Maternity Survey 2014).
With up to 60% of mothers open to natural birth now is the time to consider making this safe, effective, low cost option more widely available.

On land mothers contend with the force of gravity which limits movement as labour progresses and they tire.
Many women do not have the fitness to maintain upright postures for lengths of time. (Gupta JK, Hofmeyr GJ, Smyth R 2007).
Mothers who are overweight or obese are often unable to cope with the physical demands.

The transition from the land to water helps revive & energise mothers giving them a new lease on life and sense of purpose.
The buoyancy of water supports the mother reducing her relative weight by approx. 33% (Archimedes Principle).
This allows her to move in ways not possible on land.
To explore and benefit from the postures natural to labour & birth .

The calming, relaxing effect of the warm water promotes the flow of oxytocin.
This powerful hormone plays a huge role in childbirth.
It causes the uterus to contract and triggers the ‘fetal ejection reflex’.
Immersion in water has a beneficial physiological effect on hormone secretion, including oxytocin surges which can advance dilation and stimulate contractions (Odent 2014).
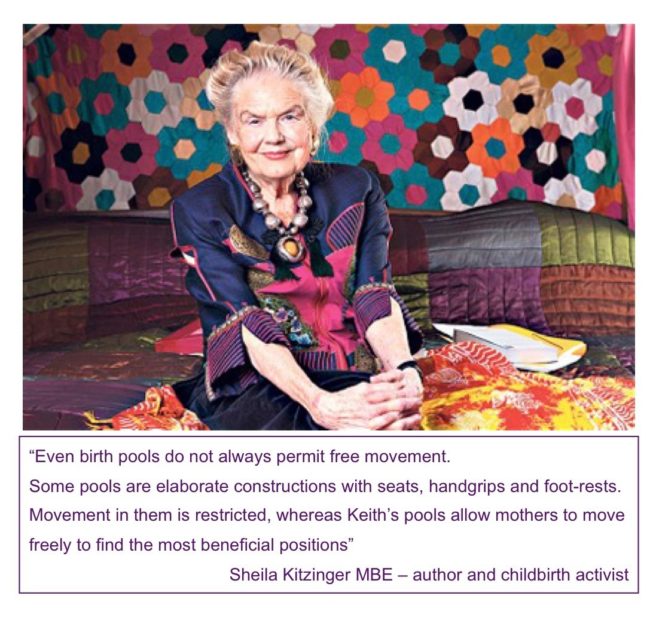
Introduksjon til Active II/360 Fødselsbasseng med Tilpasset Vannsøyle: Et Høydepunkt av Innovasjon innen Fødselsomsorg
Active Birth Pools tilbyr Active II/360 Fødselsbasseng med Tilpasset Vannsøyle, en sofistikert løsning skreddersydd for helseinstitusjoner som streber etter å tilby eksemplarisk fødselsomsorg.
Denne avanserte kombinasjonen integrerer et toppmoderne fødselsbasseng med en funksjonell og stilig vannsøyle, som er selve symbolet på det siste innen designinnovasjon og materialteknologi for fødselsomsorgssektoren.
Avansert Utvikling for Moderne Helsebehov
Active II/360 Fødselsbasseng, et produkt fra Active Birth Pools, er designet for å møte de utviklende kravene til moderne fødselsomsorg.
Sammen med den Tilpassede Vannsøylen er dette systemet resultatet av omfattende forskning og samarbeid med helsepersonell.
Fokuset har vært på å skape en løsning som tilbyr overlegen funksjonalitet, sikkerhet og komfort, samtidig som det også dekker de praktiske behovene til både helsepersonell og mødre.

Ergonomisk Design for Forbedret Opplevelse
Active II/360 Fødselsbasseng er designet med vekt på ergonomisk utmerkelse og romeffektivitet.
Bassengs nøkkelhullsform er ikke bare visuelt tiltalende, men tilbyr også funksjonelle fordeler, som støtter en rekke fødselsposisjoner og bevegelser.
Bassenget inkluderer nedsenkede håndtak og en okselignende kant for ekstra støtte og sikkerhet.
Den Tilpassede Vannsøylen er sømløst integrert, som tilbyr en elegant løsning for nødvendig rørleggerarbeid og armaturer, og dermed forbedrer bassengets nytte og estetikk.

Overlegen Materialkvalitet
Konstruert fra Ficore®, et proprietært komposittmateriale eksklusivt for Active Birth Pools, tilbyr Active II/360 eksepsjonell holdbarhet, hygiene og sikkerhet.
Materialets høyt polerte, ultraglatte overflate er mindre glatt, avgjørende for å sikre sikkerhet.
Vannsøylen, laget av det samme kvalitetsmaterialet, komplementerer bassengets design og opprettholder de høye hygienestandardene som kreves i helsemiljøer.

Brukersentrerte Funksjoner
Active II/360 Fødselsbasseng med Vannsøylen inkluderer et støttesete for arbeid, som letter optimal fødselsposisjonering og komfort for moren og et sete på kantenivå for overvåking og nødevakueringer.
Bassengdesignen muliggjør fri bevegelse, som er essensielt for effektiv bruk av vannimmersion under arbeid.
Vannsøylen tilfører funksjonalitet som en stabil støttestruktur og en praktisk nytteplattform.

Integrerte Teknologiske Forbedringer
Bassenget er utstyrt med flerfarget LED-belysning og Bluetooth lydsystemer, som muliggjør skapingen av et personlig og beroligende miljø.
Disse funksjonene er integrert i å etablere en støttende atmosfære som er gunstig for naturlig fødsel.

Bærekraft og Økonomiske Fordeler
Det holdbare designet av Active II/360 Fødselsbasseng med Tilpasset Vannsøyle gjør det til et bærekraftig og økonomisk fornuftig valg for helseinstitusjoner.
Dens langvarige ytelse og reduserte erstatningskrav gjør det til en effektiv investering, i tråd med de økonomiske og miljømessige målene til moderne helseinstitusjoner.

Produktdatablad
Active II/360 Fødselsbasseng med Tilpasset Vannsøyle har blitt anerkjent globalt for sin innovative tilnærming til fødselsomsorg.
Dens adopsjon av helseinstitusjoner over hele verden er et testament til dets effektivitet, pålitelighet og forpliktelse til å fremme vannfødselspraksiser.
Avslutningsvis representerer Active II/360 Fødselsbasseng med Tilpasset Vannsøyle fra Active Birth Pools en harmonisk blanding av avansert design, overlegen materialteknologi og gjennomtenkt integrering av brukersentrerte funksjoner.
Det står som et strategisk og innovativt valg for helseinstitusjoner som ser etter å tilby en overlegen fødselsomsorgsopplevelse, som tilbyr komfort, sikkerhet og effektivitet i en omfattende og elegant pakke.
Active II/360 Water Birth Pool – Produktdatabladt

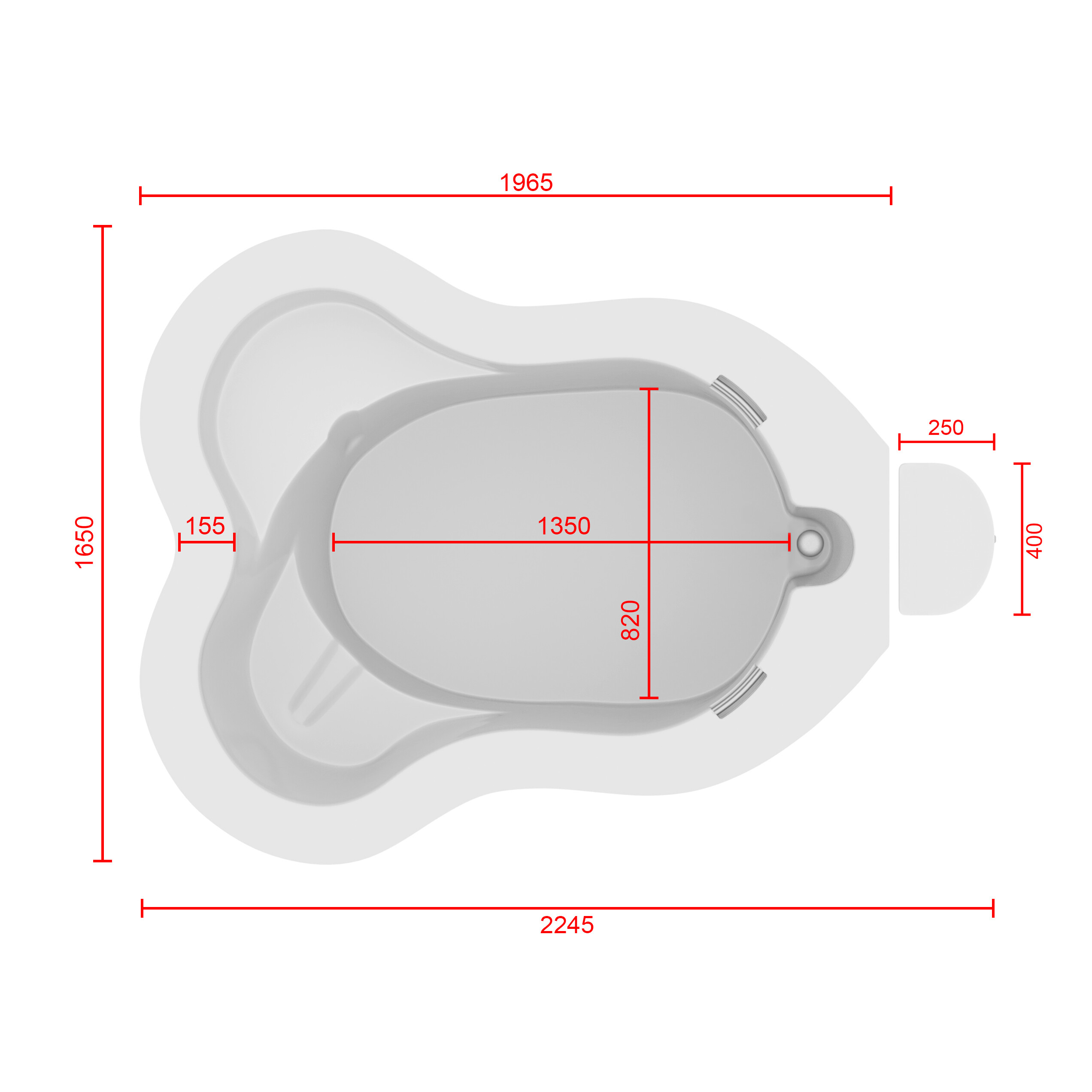

Plasser markøren din på modellen nedenfor for å flytte bildet rundt.
For å se hvordan Active II/360 Fødselsbasseng ville se ut i ditt føderom, klikk på banneret nedenfor med telefonen eller nettbrettet ditt.
High BMI Waterbirth – time for trusts to take the plunge?
Water births provide ‘clear benefits’ for healthy mums and their newborns, with fewer complications
July, 6, 2022
I News – Paul Gallagher – health Correspondent
Compared with standard care, a water birth significantly reduced the use of epidurals as well as pain and heavy bleeding after the birth, researchers found
Data analysis of the study results showed that a water birth, regardless of whether women birth in or out of the pool, ‘has clear benefits to women’ in obstetric units, where most births take place (Photo: Darlene Pfister/Star Tribune/Getty)
Water births provide “clear benefits” for healthy mothers and their newborns, with fewer interventions and complications during and after the birth than standard care, researchers believe.
Analysis of the available evidence also found that water births result in higher levels of satisfaction for mothers. A water birth involves using a birthing pool to achieve relaxation and pain relief, either exiting the pool for the birth, so the baby can emerge into air to breathe, or remaining in the birthing pool for the birth, bringing the baby to the surface to start breathing.
The Oxford Brookes University researchers compared the extent of healthcare interventions needed during and after labour between the two different types of water birth and to see if outcomes differed between a water birth and standard care – without the use of a birthing pool. They analysed 36 studies published between 2000 and 2021 involving 157,546 women.
The studies included a broad range of interventions and outcomes, including induced labour, artificial breaking of waters, stimulation of labour and epidural use among many others.
Data analysis of the study results showed that a water birth, regardless of whether women birth in or out of the pool, “has clear benefits to women” in obstetric units, where most births take place and where healthcare interventions and complications are more probable than in midwife-led units, note the researchers. A water birth was as safe as standard care for healthy mums and their newborns.
Compared with standard care, a water birth significantly reduced the use of epidurals, injected opioids, episiotomy, as well as pain and heavy bleeding after the birth. And it increased mothers’ satisfaction levels and the odds of an intact perineum. And there was no difference in the rate of C-sections, the Oxford Brookes University researchers found.
“Water immersion can significantly increase the likelihood of an intact perineum and reduce episiotomy, an intervention which offers no perineal or fetal benefit, can increase postnatal pain, anxiety, and impact negatively on a woman’s birth experience,” they concluded.
There were more instances of umbilical cord breakage among water births, but the rate was still low: 4.3/1000 births in water compared with 1.3/1000 births with standard care. This may be linked to pulling on the umbilical cord when the newborn is brought up out of the water, the researchers suggested.
They acknowledge that information on birth settings, care practices, interventions and outcomes varied considerably among the studies, and few were carried out in midwife-led units or in the mother’s home, which may have affected the findings of analysis.
But they conclude: “Water immersion provides benefits for the mother and newborn when used in the obstetric setting, making water immersion a low-tech intervention for improving quality and satisfaction with care.
“In addition, water immersion during labour and water birth alter clinical practice, resulting in less augmentation, episiotomy, and requirements for pharmacological analgesia. Water immersion is an effective method to reduce pain in labour, without increasing risk.”
The researchers, who publish their findings in the journal BMJ Open, called for future research to include factors that are known to influence interventions and outcomes during and after labour and birth. These include how many children a woman has already had, where she gives birth, who looks after her, and the care she receives, they said.
احتضان المد: الحالة المقنعة لحمامات المياه خلال الولادة في المستشفيات
في الساحة المتطورة باستمرار لرعاية الأمومة، تسعى المستشفيات باستمرار إلى وسائل مبتكرة لتعزيز تجربة الولادة للأمهات المتوقعات. إحدى هذه الابتكارات التي تكتسب قوة هي دمج حمامات المياه خلال مرافق المستشفيات. بعيدًا عن أن تكون مجرد اتجاهٍ، تقدم حمامات المياه للولادة فوائد كثيرة لا تقتصر فقط على أولياء الأمور ولكن تساهم أيضًا في تحسين تجربة الولادة بشكل شامل وتعزيز الشعور بالتمكين. في هذا المقال، سنتناول الأسباب المقنعة التي يجب على المستشفيات أن تفكر في اعتناق هذا التوجه ودمج حمامات المياه في خدمات رعاية الأمومة الخاصة بها.

تخفيف الألم بشكل طبيعي:
لقد تم التعرف على الماء منذ فترة طويلة كمسكن طبيعي قوي. الانغماس في الماء الدافئ يمكن أن يخفف من شدة التقلصات ويوفر إحساسًا بعدم الوزن، مما يقلل من تأثير الجاذبية على الجسم. تقدم المستشفيات التي توفر حمامات المياه للولادة للأمهات خيار إدارة الألم البديل الذي يكمل الطرق التقليدية، مما يوفر نهجًا أكثر شخصنة للراحة خلال الولادة. أظهرت العديد من الدراسات فعالية الانغماس في الماء في تخفيف ألم الولادة. خلصت مراجعة نشرت في “مجلة التعليم الأمومي” (هاربر وآخرون، 2016) إلى أن الانغماس في الماء الدافئ أثناء الولادة يقلل بشكل كبير من تصور الألم، مما يوفر للأمهات المتوقعات خيارًا لتخفيف الألم غير دوائي ومستند إلى الأدلة. تشير الأبحاث المنشورة في “مجلة التمريض النسائي والتوليدي وحديثي الولادة” (ثويني وآخرون، 2019) إلى أن الانغماس في الماء أثناء الولادة يقلل من هرمونات التوتر، مما يعزز حالة أكثر استرخاءً للأم والطفل. ربط انخفاض مستويات هرمونات التوتر بتحسين الرفاهية الأمومية والنتائج المواتية للولادة، مما يدعم الحجة لحمامات المياه كنهج شامل لرعاية الأمومة.

تقليل التوتر والقلق:
يمكن أن يكون عملية الولادة مصدر قلق للعديد من الأمهات المتوقعات. تخلق حمامات المياه للولادة بيئة هادئة ومهدئة، تعزز الاسترخاء وتقلل من مستويات التوتر. تعزز الطفو في الماء إحساسًا بعدم الوزن، مما يسمح للأمهات بالحركة بحرية أكبر وتبني وضعيات مريحة، مما يسهم في تجربة ولادة إيجابية وممكنة بشكل أكبر. تشير الأبحاث المنشورة في “مجلة التمريض النسائي والتوليدي وحديثي الولادة” (ثويني وآخرون، 2019) إلى أن الانغماس في الماء أثناء الولادة يقلل من هرمونات التوتر، مما يعزز حالة أكثر استرخاءً للأم والطفل. رُبطت مستويات منخفضة لهرمونات التوتر بتحسين الرفاهية الأمومية والنتائج المواتية للولادة، مما يدعم الحجة لحمامات المياه كنهج شامل لرعاية الأمومة.

تسهيل الحركة والتوجيه:
توفر حمامات المياه للولادة بيئة تسهل الحركة والتوجيه خلال عملية الولادة. يسمح الطفو بزيادة القدرة على الحركة، مما يتيح للأمهات تغيير وضعياتهن بسهولة والعثور على أكثر وضع مريح للولادة. يمكن أن تعزز هذه المرونة تقدم عملية الولادة وتسهل عملية الولادة. أظهرت دراسة نشرت في “المجلة الأمريكية لطب النساء والتوليد” (زانيتي-دالينباخ وآخرون، 2007) أن الانغماس في الماء يعزز القدرة على الحركة لدى الأمهات خلال الولادة. يسمح طفو الماء بحركة وتوجيه أسهل، مما قد يقلل من مدة الولادة ويقلل من الحاجة إلى التدخلات. تؤكد هذه الأدلة على أهمية حمامات المياه في توفير بيئة تسهل التوجيه الأمثل لعملية الولادة.

تحسين الدورة الدموية:
الماء الدافئ في حمام الولادة يعزز تحسين الدورة الدموية، وهو ما يمكن أن يكون مفيدًا بشكل خاص خلال عملية الولادة. تساعد التداول المحسّن في التقليل من الانتفاخ وتعزيز تدفق الأكسجين، مما يسهم في رفاهية الأم والطفل على حد سواء. تعتبر المستشفيات التي تدمج حمامات المياه للولادة أولوية للجوانب الفسيولوجية للولادة، معززة بذلك بيئة ولادة أكثر صحة. لقد تم توثيق التأثير الإيجابي للانغماس في الماء الدافئ على الدورة الدموية بشكل جيد. أظهرت دراسة سيطرية عشوائية نشرت في “مجلة القابلات وصحة المرأة” (بيرنز وآخرون، 2012) أن الانغماس في الماء الدافئ يزيد من تدفق الدم في الأطراف وتأكسجها، مما يوفر فوائد فسيولوجية تسهم في الرفاه العام للأم والطفل.

تعزيز الرباط:
الإعداد الحميم والخاص لحمام الولادة يشجع على مشاركة الشريك ويعزز الرباط الأعمق بين الآباء والمولود الجديد. تجربة الولادة المشتركة في حمام الولادة يمكن أن تعزز الرابط العاطفي بين الشركاء، معززةً الشعور بالوحدة والمسؤولية المشتركة في استقبال أحدث أفراد العائلة. أجريت دراسة شاملة للميتا نشرت في “مجلة الولادة: قضايا الرعاية خلال فترة ما بعد الولادة” (نيكوديم وآخرون، 2016) لفحص النتائج النفسية للانغماس في الماء أثناء الولادة. أظهر التحليل وجود ترابط إيجابي بين تجارب الولادة في الماء وزيادة الرضا الأمومي والرباط مع المولود الجديد.

ختام:
المستشفيات التي تعتبر إدماج حمامات المياه للولادة أولوية تتماشى مع الأدلة التي تدعم الفوائد العاطفية لهذا النهج في الولادة. إدماج حمامات المياه في خدمات الرعاية بالمستشفى للأمومة يمثل خطوة تقدمية نحو توفير نهج أكثر شمولًا وتركيزًا على المريض في عملية الولادة. فوق الفوائد الجسدية، مثل تخفيف الألم الطبيعي وتحسين الدورة الدموية، تساهم حمامات المياه للولادة في تحسين تجربة عاطفية أكثر غنى للوالدين. مع سعي المستشفيات للأولوية لرفاهية وتفضيلات الأمهات المتوقعات، يظهر إدماج حمامات المياه كخيار مقنع، مستذكرًا الارتباط القديم بين الإنسانية وضمان الماء المهدئ خلال معجزة الولادة. إدماج حمامات المياه في خدمات الرعاية بالمستشفى للأمومة ليس مجرد خطوة تقدمية؛ بل هو قفزة مدعومة علميا نحو توفير تجارب الولادة القائمة على الأدلة ومحورة حول المريض. تعزيز فوائد الانغماس في الماء خلال الولادة من خلال العديد من الدراسات يعزز الفكرة بأنه يجب على المستشفيات أن تعتبر حمامات المياه للولادة ليست فاخرة بل عنصرًا حيويًا في تعزيز بيئة ولادة آمنة ومريحة وقائمة على الأدلة. إن جمود الأدلة يدعم بقوة إدماج حمامات المياه كقوة محولة في رعاية الأمومة الحديثة.
Birthing Pool Rules: Journal of Water Safety Forum Spring 2021
Water births are largely considered safe — but are there potential microbiological risks? And what are the best recommendations to eliminate any possible dangers?
Dr Jimmy Walker clarifies some of the advice outlined in an upcoming ‘back to basics’ book* aimed at training and education on the potential microbiological risks from water in healthcare facilities.
Water births have long been considered a safe way of giving birth for women who are not expected to have complex deliveries, with the literature backing up this record to show that rates of neonatal infections are no greater in water births than conventional bed births.1,2,3,4
However, this doesn’t mean there are no risks at all. Rare instances of adverse events have occurred, including microbial neonatal infections caused by a range of organisms that have included Legionella, the cause of Legionnaires’ disease, and Pseudomonas aeruginosa — although these have largely been related to home births.
There are several routes for potential contamination of water during a water birth:
Water supply
If either of the above organisms were found in a pool, this would indicate either contamination in the water system or at the tap outlet. If only a tap outlet were colonised, the contamination may be diluted to negligible levels in the pool once that tap is run. However, running a tap when there is biofilm build-up, either in the last two metres or further back in the system, would continue to release microorganisms leading to microbial concentrations in the pool water that could lead to infections.
This is a highly unlikely scenario that would only occur if water maintenance has been neglected enough to allow conditions for microbial growth to develop: for example where pipes have not been lagged properly causing the hot water to become cooler and the cold pipe to become warmer, creating ideal temperatures to enable growth of Legionella bacteria, for example.
Bodily fluids, birthing ‘debris’ and maternal contamination
As part of the birth process, water in birthing pools will inevitably be contaminated by bodily fluids and ‘debris’, such as placenta, some of which will be caught in strainers. Pool water can also be contaminated by faecal matter and any P. aeruginosa the mother may be carrying (P. aeruginosa can occur naturally on the skin of healthy individuals), although newborns are unlikely to be at risk from maternal ‘flora’.
A clear protocol is essential for drainage of the pool, cleaning and also disinfection to remove this contamination. All accessories must also be cleaned and thoroughly disinfected — or be single use.
If contamination is not properly dealt with, then any remaining residues will encourage microbial growth that could lead to potentially dangerous contamination of the next user’s water.
Drains
The role of drains as a source of healthcare associated infections (HAIs) and potential reservoirs of antibiotic resistant organisms is now being regularly documented, with carbapenem-resistant Enterobacteriaceae (CREs) a particular concern.
Single use plugs and strainers are now most commonly used, with a large access valve for nurses and midwives to retain water in the bath. However, because birthing pools are usually located at floor level, the gradient of the drainage pipework may not be sufficient to remove the material caught in the drain. Although such an event has not yet been reported, this creates the potential for biofilmbuild-up over time, to a level that may be difficult for disinfectants to penetrate and possible contamination of the pool as soon as it is filled.
Birthing pool design
Birthing pools could be improved to prevent this backflow scenario from the drain, with designs that ensure efficient drainage of contaminating material and valves and drains that are easy to disinfect.
There are also examples of birthing pools where the pool is filled via a wall tap that enters the pool at a level where the water could flow back into the tap. This again has the potential for back contamination of the tap, with bacterial colonisation reaching even further back into the system in contravention of the water fitting directive.
Birthing pools should be designed with taps that are well above the pool’s edge and which are fitted with suitable backflow protection.
Some birthing pools also have an associated showerhead for cleaning the pool after use. However, this is also inadvisable as the flexible hose and shower head may become contaminated when they are suspended in the water. This could not only lead to backflow and contamination of the supply, but also, the contaminated hose and shower head could introduce harmful bacteria to the pool if they are not cleaned and disinfected appropriately or replaced between uses.
In addition, because water births are not always considered appropriate, there may be a prolonged period when the pool is not used. Where this is the case, a flushing regime is essential to minimise water stagnation, biofilm build-up and microbial proliferation in the water supply.
Resolving issues
Maternity units are well aware of the risks and must carry out their own risk assessments, but it is important that they are assisted in this by appropriate members of the hospitals’ water safety groups (WSGs – see p 10-12), who can provide additional specialist knowledge e.g. from microbiologists and the estates team.
Health Building Note 09-02 provides regulations and recommendations for birthing pools
References
- Thoeni, A. et al “Review of 1600 water births. Does water birth increase the risk of neonatal infection?” J Matern Fetal Neonatal Med 17: 357–361, 2005. “https://doi.org/10.1080/14767050500140388″doi.org/10.1080/14767050500140388
- Neiman, E. et al “Outcomes of water birth in a US hospital-based midwifery practice: A retrospective cohort study of water immersion during labour and birth”, J Midwifery Womens Health 65:216–223, 2020. “https://doi.org/10.1111/jmwh.13033″/doi.org/10.1111/jmwh.13033
- Bovbjerg, M.L., Cheyney, M., Everson, C. “Maternal and newborn outcomes following waterbirth: The midwives alliance of North America statistics project, 2004 to 2009 Cohort, J Midwifery Womens Health 61:11–20, 2016. “https://doi.org/10.1111/jmwh.12394″doi.org/10.1111/jmwh.12394
- 4. Taylor, H. et al “Neonatal outcomes of water birth: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal 101(4):357-365, 2016. doi.org/10.1136/archdischild-2015-309600
RCM welcomes research showing benefits of water birth
RCM welcomes research showing benefits of water birth
06 July 2022
RCM Maternity Services Midwifery Workforce Midwife Shortage MSWs – Maternity Support Workers Staffing Levels Waterbirth
Research showing the safety and positive benefits for women having a water birth has been welcomed by the Royal College of Midwives (RCM). The research showed that women having a water birth in a hospital obstetric unit had fewer medical interventions and complications during and after the birth.
Commenting on the research, Clare Livingstone, Professional Policy Advisor at the RCM, said: “This is really good news for women choosing to have a water birth or thinking of having one. There has been previous research outlining the benefits for women and this significant study adds weight to those. It is also positive because it is more information for women when deciding how they want to give birth.
“Water births are becoming more widely available for women across the UK, but this isn’t the case everywhere. The challenge now is to ensure this choice is open to all women wherever they live.”
The study did show a small increase in ‘umbilical cord snaps’ – where the baby’s umbilical cord breaks – though the rates remain very low. This will not hurt the baby and the midwife will respond quickly and clamp the cord to prevent any bleeding.
Clare Livingstone added, “What is needed now is to see more research into water births in midwife led settings and in women’s homes. This will give us a broader picture of the impact of water births across all the places in which women give birth.”
The research from Oxford Brookes University will be published in the open access journal BMJ Open tomorrow (6 July).
The Oxford Brookes University research can be read at https://bmjopen.bmj.com/content/12/7/e056517.full.
The Royal College of Midwives (RCM) is the only trade union and professional association dedicated to serving midwifery and the whole midwifery team. We provide workplace advice and support, professional and clinical guidance, and information, and learning opportunities with our broad range of events, conferences, and online resources. For more information visit the RCM | A professional organisation and trade union dedicated to serving the whole midwifery team.
The use of water for labour and birth
Health Times: Karen Keast
Water is a life force in more ways than one – it covers more than 70 per cent of our earth and we drink it to survive.
When it comes to using water for childbirth, water birth is still a contentious issue that divides healthcare professionals and organisations alike.
The fact that it’s contentious at all surprises some of Australia’s leading midwives, writes Karen Keast.
There are legends of Egyptian pharaohs being born in water and of South Pacific women giving birth in shallow seas.
The first written report of a water birth in the western world occurred in France in 1803, when a mother experiencing a long and difficult labour was helped to give birth in a tub of warm water.
In the 1970s, Igor Tjarkovsky, a boat builder, investigated the therapeutic benefits of water and installed a glass tank in his home for women to use for childbirth.
French obstetrician Michel Odent went on to pave the future of water birth.
After a mother, using water to ease the pain of her labour, accidentally gave birth in the water, he went on to install a plastic paddling pool in a hospital so more women could enjoy the benefits of water birth while reducing their need for painkillers.
Only a small proportion of women in Australia choose to give birth in water each year although the exact number of water births is not known.
Griffith University Professor Jenny Gamble, a practising midwife of 30 years, says water births have come a long way in Australia but there is still a long way to go.
Professor Gamble recalls when a new maternity wing opened up at a Brisbane hospital, the then director general who was touring the facility instructed the plugs from the tubs to be removed.
“In his own way, he was saying water births might be a bad thing,” she says.
“Those days are gone. Water has become more accessible to women. There’s quite a lot of evidence to say that water is safe for women.
“More and more hospitals are putting in big tubs and there’s a range of deep tubs. It’s coming but it’s all too slow.”
Advocates of water birth say its benefits include the relaxing effect of warm water and feelings of weightlessness, buoyancy and ease of movement which help to alleviate pain naturally.
Western Sydney University Professor Hannah Dahlen, a privately practising midwife and spokesperson for the Australian College of Midwives, says evidence shows water immersion may also help improve blood flow in the uterus, lower blood pressure, provide less painful contractions and result in shorter labours and fewer interventions.
Professor Dahlen last year published a study in the Journal of Midwifery examining the outcomes of 6144 Australian women who had normal vaginal births in a birth centre over a 12-year period.
Her research compared women giving birth in water with those who gave birth in six other positions out of the water – kneeling or all fours, squatting, side lying, using a birth stool, standing and, the most common birth position in the country – semi-seated.
Professor Dahlen found those who gave birth on a birth stool had almost a one-and-a-half time’s higher rate of major perineal trauma and more than twice the rate of haemorrhage after delivery compared with water birth.
There was no difference in major perineal trauma and haemorrhage after delivery between women who gave birth in water and those who had a semi-seated position.
While those babies born in a semi-seated position had a four-and-a-half time’s higher incidence of five minute APGAR scores less than seven.
APGAR scores, which rate the newborn’s breathing effort, heart rate, muscle tone, reflexes and skin colour, of less than seven at five minutes after birth indicate medical intervention was needed to resuscitate the baby.
“Some studies have shown better outcomes but basically I found no difference to other birth positions,” she says.
“There was no evidence of harm. We want to do more research in Australia.
“We have no evidence to date that it’s harmful but we need more and more evidence to show it’s safe.”
Professor Dahlen says a water birth also provides women with a sense of protected space.
“They talk about how they felt there was a barrier; they felt it was a cocoon where they could feel safe,” she says.
Professor Dahlen says one common concern about water births is that the baby could drown but she says babies are born with a diving reflex, or bradycardic response, that causes them to hold their breath under water.
Professor Dahlen says despite mounting evidence proving the benefits of water birth, they still remain contentious in Australia.
“I have never understood it. I find it fascinating that water is so scary.”
Professor Gamble agrees.
“We’re talking about water, just water – not epidurals, not heavy duty drugs,” she says.
“Thank goodness hospitals are moving towards increasing their remodelling of their maternity suites to include tubs but quite frankly it’s a lot of fuss for something as simple as warm water.”
Professor Gamble says water births are common practice at planned home births, and are used during labour or active birth.
“Some women want to get in and get out for birth, some want to labour in the water and some hop in just for the birth – anything goes.”
Perhaps, most importantly, Professor Dahlen says water births are not about the baby.
“That’s what people get wrong,” she says.
“It’s about the mother and if you have a really happy and relaxed and stress free mother you actually have a baby that’s advantaged – they are born and very placid.
“They don’t often cry – they come up and blink.
“They are breathing fine. They come up all lovely and warm and then go to their mother’s chest.
“I really love water births.”
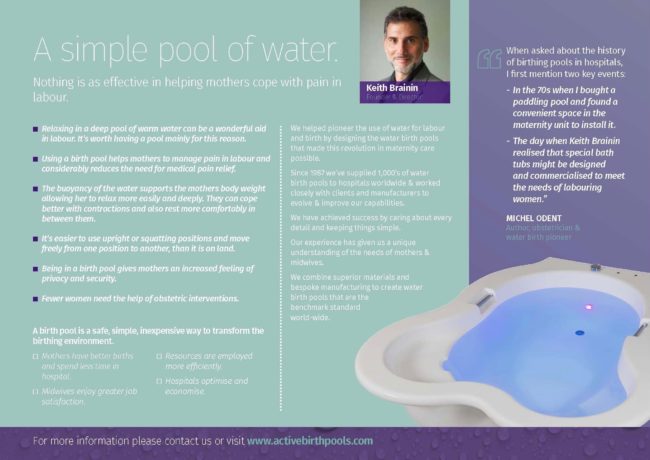
Giving birth in water: Low risk, high reward – study
Researchers concluded that water birth is as safe as standard intrapartum care for healthy individuals, and can reduce physical pain as well as anxiety during labor.
Water births have undeniable benefits for expectant parents and new babies, according to a study published on Tuesday in BMJ Open.
The peer-reviewed study comes out of Oxford Brookes University in the United Kingdom, in conjunction with researchers at Emory University (Georgia, US) and the University of Nevada Las Vegas (Nevada, US).
The study
For the purposes of the study, any birth that involved using a birthing pool for relaxation and pain relief was considered a water birth, even if the infant’s entrance into the world did not physically occur in the water. This is to say, those who labored in a birthing pool and then gave birth outside the pool were also counted among the data.
The history of Water Birth
There have been accounts of women labouring and giving birth in water mostly amongst peoples living near a source of shallow warm water such as the South Pacific islanders.
In most traditional societies the rituals and practices of childbirth have, until recent times, been a matter of secrecy and handed down through generations of women.
There are oral traditions of similar practices among the Maori, the Indians of Central America, and the Ancient Greeks and Egyptians.

In 1805, the first account the use of water in Europe was documented.
A French woman, who had laboured for two days before being encouraged to get into a warm bath by her enlightened doctor then progressed to give birth to a healthy baby within an hour.
Sadly, for millions of women at the time there was no recognition of the importance of this event.
Aside from this, there are no accounts of a tradition of childbirth in water in Europe or other northerly regions.
The reason for this may be a simple matter of climate and plumbing.
Only with the widespread availability of artificially heated water and portable and installed birthing pools in comparatively recent times, has giving birth in water become a real option for women anywhere in the world.
Waterbirth was pioneered in the 1960’s by the Russian researcher Igor Tjarkovsky.
Using a large aquarium he installed a glass tank in his own home in Moscow in which many mothers gave birth .
Stunning photographs of these extraordinary births were published in the west and inspired the first water births.
For today’s generation of mothers, the key figure in the use of water for labour and birth is the French obstetrician Michel Odent.

In 1977 Odent installed a pool in the hospital at Pithiviers , not with the idea of promoting birth in water, but primarily as an additional option for pain relief and rest during long or difficult labours.
He has said ‘the reason for the birthing pool is not to have the baby born in water but to facilitate the birth process and to reduce the need for drugs and other interventions.’
Odent published his findings in the Lancet and his recommendations in this article provided the basis for the first midwifery guidelines for waterbirths.
Odent, M. Birth under water. The Lancet. December 24/31, 1983. pp 1476-1477
Inspired by news of what was happening in Moscow and France, the earliest waterbirths in the West took place at home in pools that were often improvised by the couples themselves and attended by independent midwives.
The parents created birthing pools using any large waterproof container they could find – including refuse skips, cattle troughs, inflatable paddling pools or garden ponds lined with a plastic sheet.
This happened simultaneously in several parts of the world and began to cause ripples in the world of obstetrics.
When reports and images of the first waterbirths were published, the world looked on in amazement.
The women who chose this way of birthing and their attendants were variously regarded as crazy, deluded, foolhardy or inspired.
The medical establishment rallied to condemn or at least call the practice into question, citing theoretical risks of infection and fears of the baby drowning.
Such fears have been largely appeased by the work of Dr Paul Johnson, neonatal physiologist at the John Radcliffe Hospital, Oxford.
His research on the mechanisms that trigger breathing in the newborn provided scientific confirmation of the safety of birth underwater at body temperature for babies who are not at risk.
He described how the baby is protected against the possibility of breathing while underwater in the few seconds between emerging from the birth canal and being lifted out of the water.
This response is known as the ‘dive reflex’.
Johnson, P. Birth under water – to breathe or not to breathe. British Journal of Obstetrics and Gynaecology, vol 103, no 3, March 1996. pp 202-208

In 1999 Ruth E. Gilbert and Pat A. Tookey of the Institute of Child Health, London, published a hugely important study in the BMJ that effectively provided the ‘green light’ for labour and delivery in water.
It was a study of the outcomes for all babies born in water in the UK in a two-year period between 1994 and 1996.
A total of 4,032 waterbirths were included in the study (about 0.6 per cent of all deliveries).
All 1500 consultant paediatricians in the British Isles were asked if they knew of cases of perinatal death or admission to special care within 48 hours of labour or delivery in water.
The study showed that there was no increased risk to health for babies born in water as compared with babies born to other low-risk women on land.
Since then a burgeoning of interest in the use of water in labour in the UK has led to the development of a unique concentration of knowledge and expertise within the mainstream maternity system.
Positive encouragement to the use of water in labour and childbirth has come from the Royal College of Midwives, which recommends that midwives should develop the knowledge and skills to assist women at a waterbirth .
Water labour and birth is an option which is limited to ‘low risk’ women having an uncomplicated birth following a healthy pregnancy.
In the UK the issues of safe practice have been addressed by the health authorities, Royal College of Midwives, midwifery supervisors and one or two obstetricians.

A significant body of research studies and several important surveys have been undertaken.
Development has been more carefully and diligently monitored than many of the obstetric procedures that are widely used.
Against this backdrop, more of the managers of maternity services in the UK are increasingly being persuaded that the option of using water in labour and for birth should be available to all women.
The extent of the use of birth pools in the UK increased.
Pools are now used in hospitals as well as independent birth centres, some of which specialize in waterbirths, and in the community at home births with both independent and NHS midwives.
The Edgware Birth Centre in North London is an example of a new type of forward-thinking NHS birth unit.
Typically 70 per cent of women who give birth at the centre use water during labour and 50 per cent give birth in water.
Since it’s inception outcomes show far fewer interventions than for low-risk births at a conventional hospital birth unit.
This is a model of care which would transform our maternity services if widely adopted.
In October 2000 the UK’s Royal College of Midwives estimated that 50 per cent of maternity units provided facilities for labour or birth in water.

The usage of pool varied between 15 and 60 per cent, which may be an indicator of the significance of the role of the midwife in supporting and encouraging women to consider the use of water.
Since then the number of UK hospitals and birth centres with installed pools has risen to closer to 60 per cent.
However, that does not necessarily mean that the pools are being fully or enthusiastically utilized or that the pool is always available.
It’s not uncommon for women to be discouraged from using them or to be told that trained midwives are not available.
Sometimes stringent protocols around the use of a pool can limit it’s usefulness and frustrate both mothers and midwives.
Women who want to use a pool are often also told that this may not be possible if the pool is already in use.
It’s time for such problems to be addressed and for all women to have the possibility of using a birth pool wherever they choose to give birth.
Water birth is one of the greatest innovations in childbirth of our times and can no longer be regarded as a passing fad.
The use of epidurals today has reached epidemic proportions and contributes significantly to the high caesarean and intervention rate and is also very costly, requiring a high level of expert attendance.
The simple expedient of a pool of warm water is by now a proven way to confine the use of epidurals to those women who really need them and improve safety and quality of the birth experience.