Delivery, Moving and Handling
Mainland UK Deliveries

Active Birth Pools delivered within the mainland UK are wrapped in protective packaging and placed in double walled boxes with corrugated sides.
The pools are delivered by our dedicated carrier on a week commencing basis.
If you require delivery on a specific date or at a specific time please contact us for a quote.
Box Size and Weight
- Active Birth Pool: 1880 x 1690 x 790mm 100 kg
- Venus Birth Pool: 1960 x 1390 x 790mm 90 kg
- Princess Birth Pool: 1640 x 1140 x 790mm 80 kg
The carrier will deliver your birth pool to the receipt and distribution point.
You’ll be responsible for moving it to the room where it will be installed.
The pool should be moved from the delivery point in its cardboard box by turning it gently on its side onto a movers dolly or two.
This will enable it to be easily moved along corridors and through doorways. Once the pool is in the room where it will be installed carefully open the cardboard box and remove the protective packaging.

Outside Mainland UK and International Deliveries
Active Birth Pools that are delivered outside the mainland UK are wrapped in protective packaging and placed in timber framed crates with plywood sides that conform to ISPM15 and are stamped accordingly.
Crate Size and Weight
- Active Birth Pool: 1910 x 1720 x 890mm 200 kg
- Active II Water Birth Pool: 2050 x 1810 x 970mm 220kg
- Venus Birth Pool: 1950 x 1420 x 890mm 185 kg
- Venus II Water Birth Pool: 2050 x 1420 x 890mm 205kg
- Princess Birth Pool: 1670 x 1170 x 890mm 145 kg
The birth pool should be unpacked from the timber crate but left in its protective packaging for moving from the delivery point to the room where it will be installed.
The pool should be gently turned on its side onto a padded movers dolly or two to enable it to be easily moved along corridors and through doorways. It’s best to handle the pool by the rim as this is the strongest point.

Installation
Prior to moving the birth pool into position against the wall the plumbing (taps and drainage) and electrical services should be in place ready for final connection to the pool.
Taps
Fix a 3/4″ thermostatically controlled mixer tap with a 150mm spout on an IPS panel 25 cm above the rim of the pool (rim height 75cm).
We suggest that you consider the Rada Sense Bath T3 (or similar) as it is a digital tap that not only enables you to programme the http://activebirthpools.com/wp-content/uploads/2015/10/Rada-1.pdfwater temperature but also the fill time.
A filling time of 20 – 25 minutes is acceptable.
Drainage
The pool is supplied with a bespoke brass 40mm pop up waste that is operated by a control that is fixed to the rim.



The waste is connected to a P Trap and a McAlpine T25 adaptor
Height from the floor to the centre of the T25 adaptor is 11cm
From the T25 adaptor you can utilise of a wide variety of commonly available parts to connect to the pipework of the buildings drainage system.

When electrical and plumbing services are in place and ready for the final connection to the pool’s systems the pool should be moved into position and fixed to the floor.
Final connection of services can be carried out through the access panel when the pool is secured in place.
Fixing the birth pool to the floor
All feet MUST be in solid contact with the floor.
If the floor is not level or smooth be sure to adjust the feet or level the floor so that all of the feet are in firm contact with the floor and there is no rocking or movement.
The bottom flange of the outer panel should be in contact with the floor but is not the primary support structure of the pool and must not bear the full weight of the filled birth pool.

The water birth pool is supplied with 3 x 100 mm x 30 mm fixing brackets.
You’ll find the brackets taped to the pool just inside the access panel that can be opened with a 10mm Allen Key.
It is essential these brackets are securely fixed to the floor with suitable hardware to immobilise the pool and prevent it from moving when empty.
Failure to secure the pool to the floor with the fixing brackets will endanger the end user and VOID the guarantee.
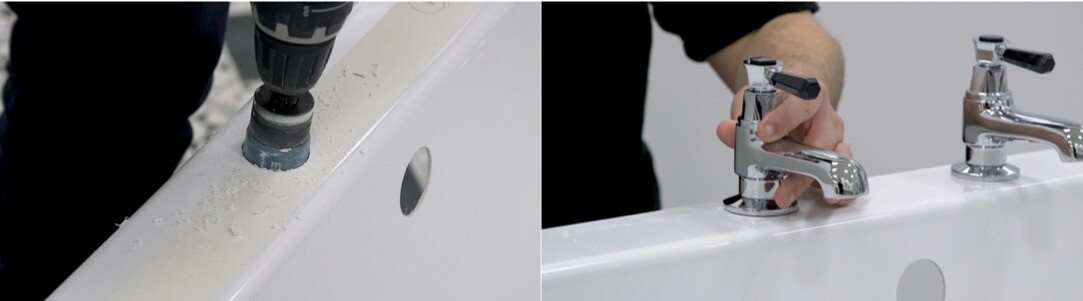
Locating and fixing the brackets
Step 1: All Models:
Mark the central position of the water birth pool on the wall that it is being fitted on.
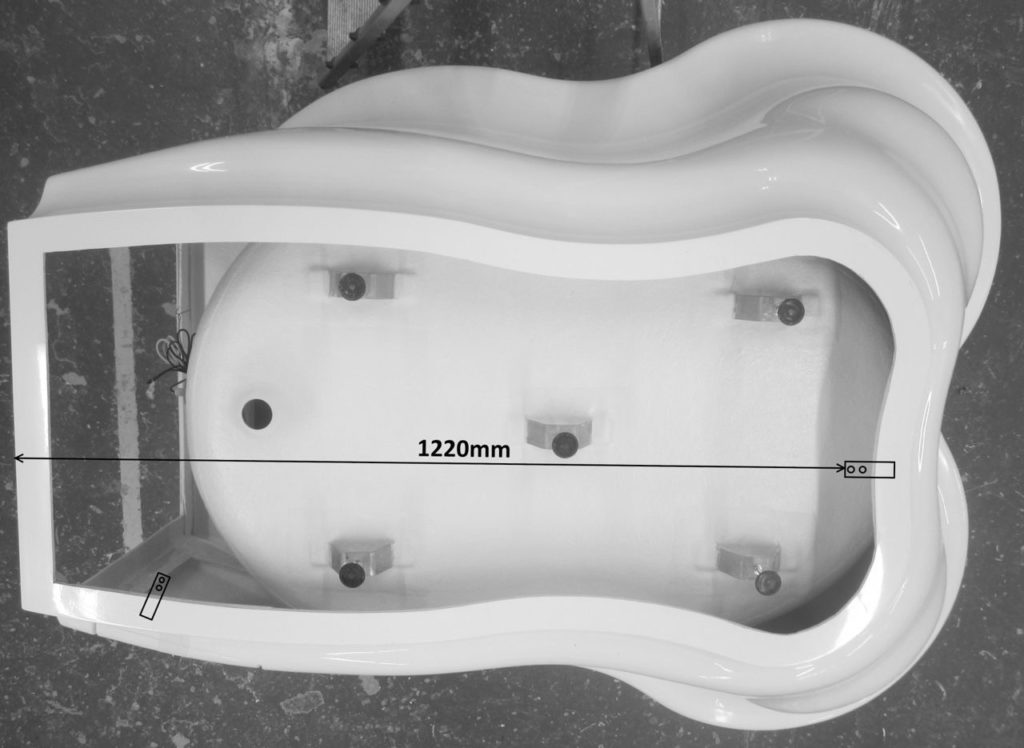
Step 2: Active Birth Pool – front fixing bracket
Measure 1220 mm from the centre point on the wall and mark this as the point to locate the bracket so that the long flat piece is projecting away from the wall and the raised short section faces forward into the room.
Fix the bracket to the floor using suitable hardware.
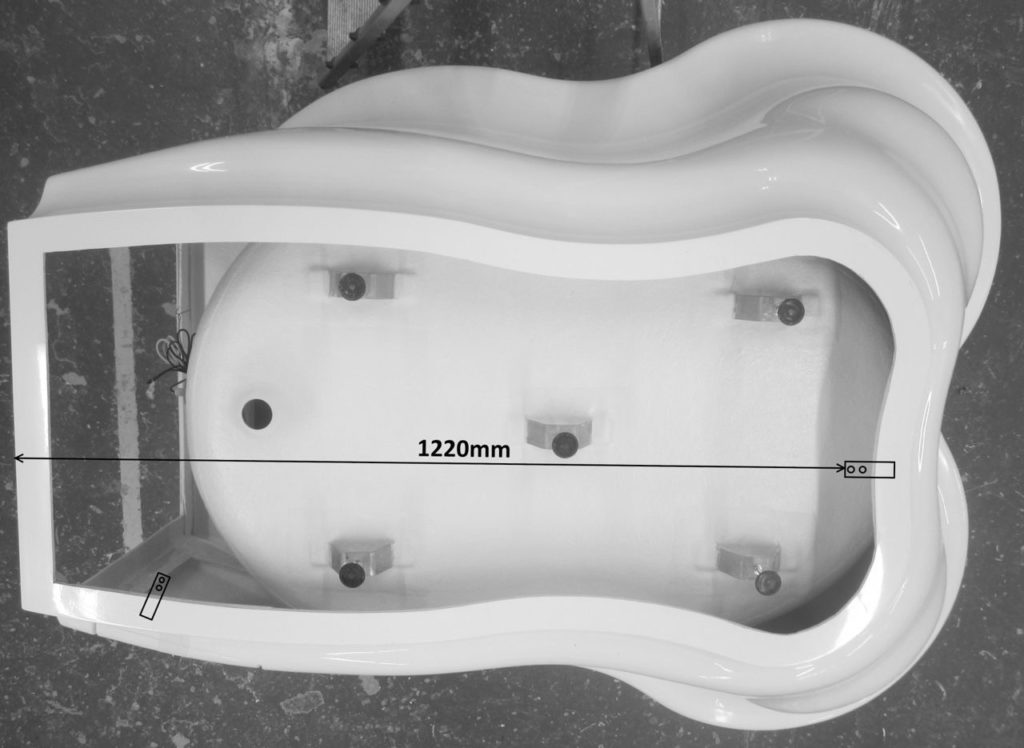
Front bracket right centre – Back bracket lower left
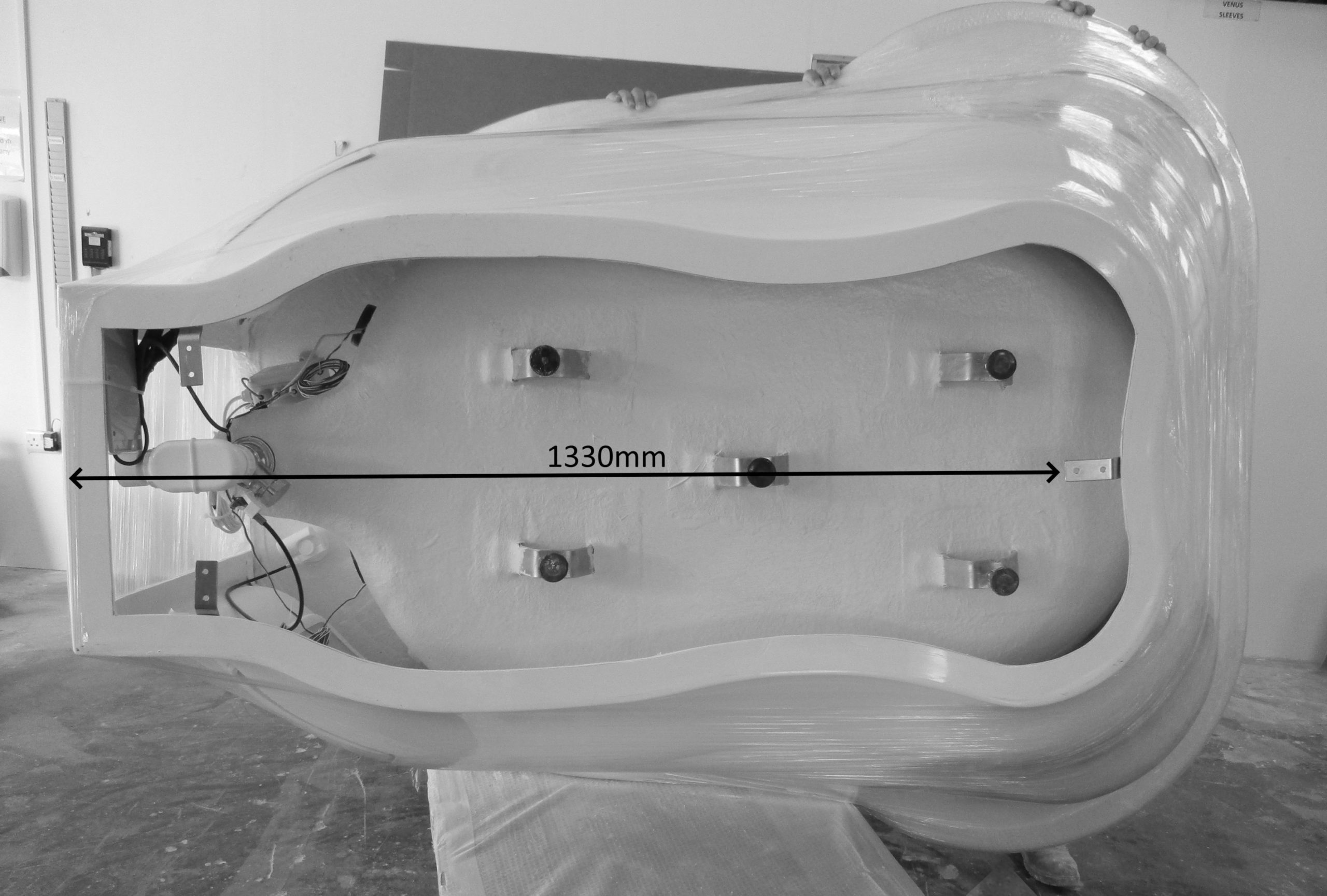
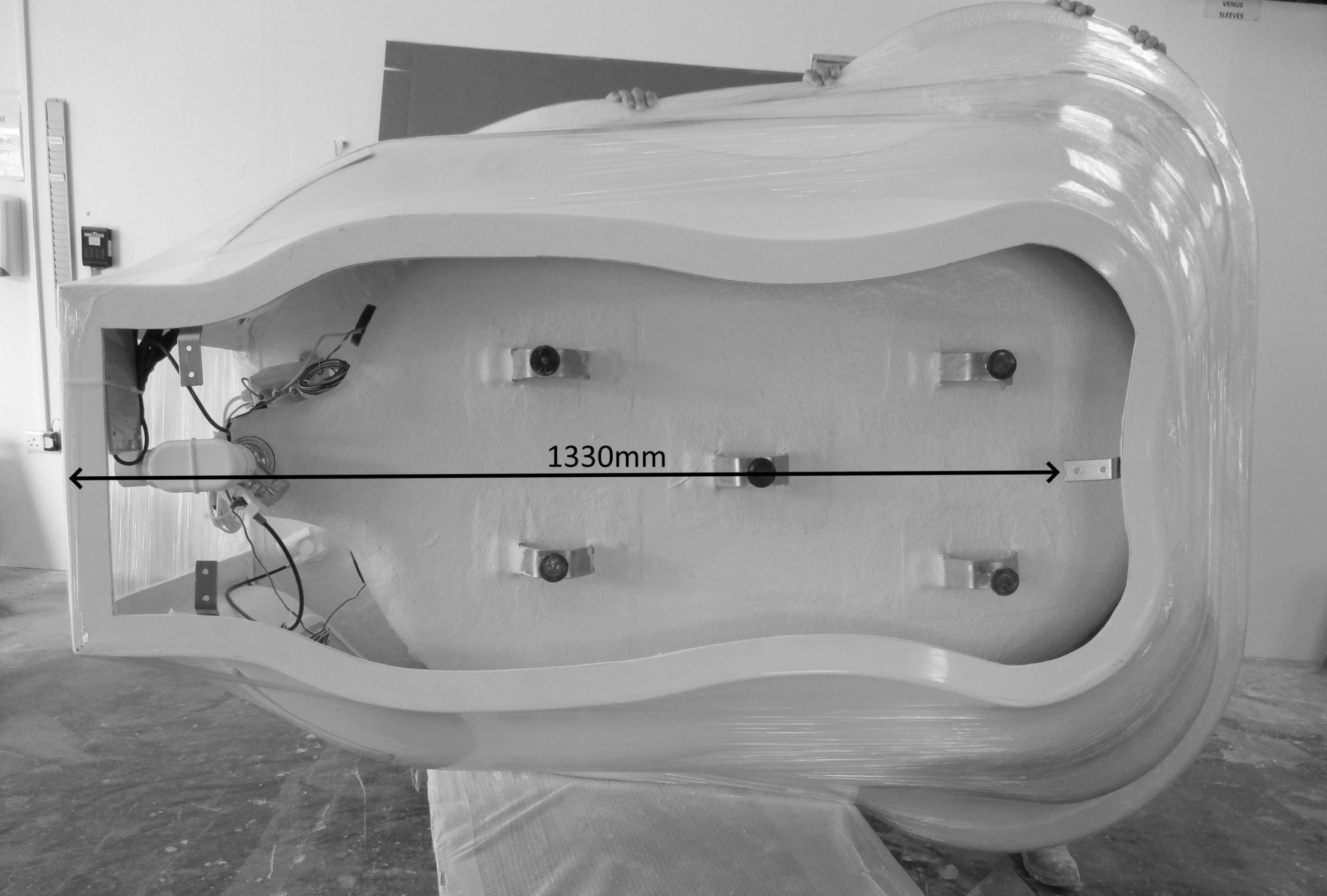
Step 2: Active II Water Birth Pool – front fixing bracket
Measure 1330 mm from the centre point on the wall and mark this as the point to locate the bracket so that the long flat piece is projecting away from the wall and the raised short section faces forward into the room.
Fix the bracket to the floor using suitable hardware.
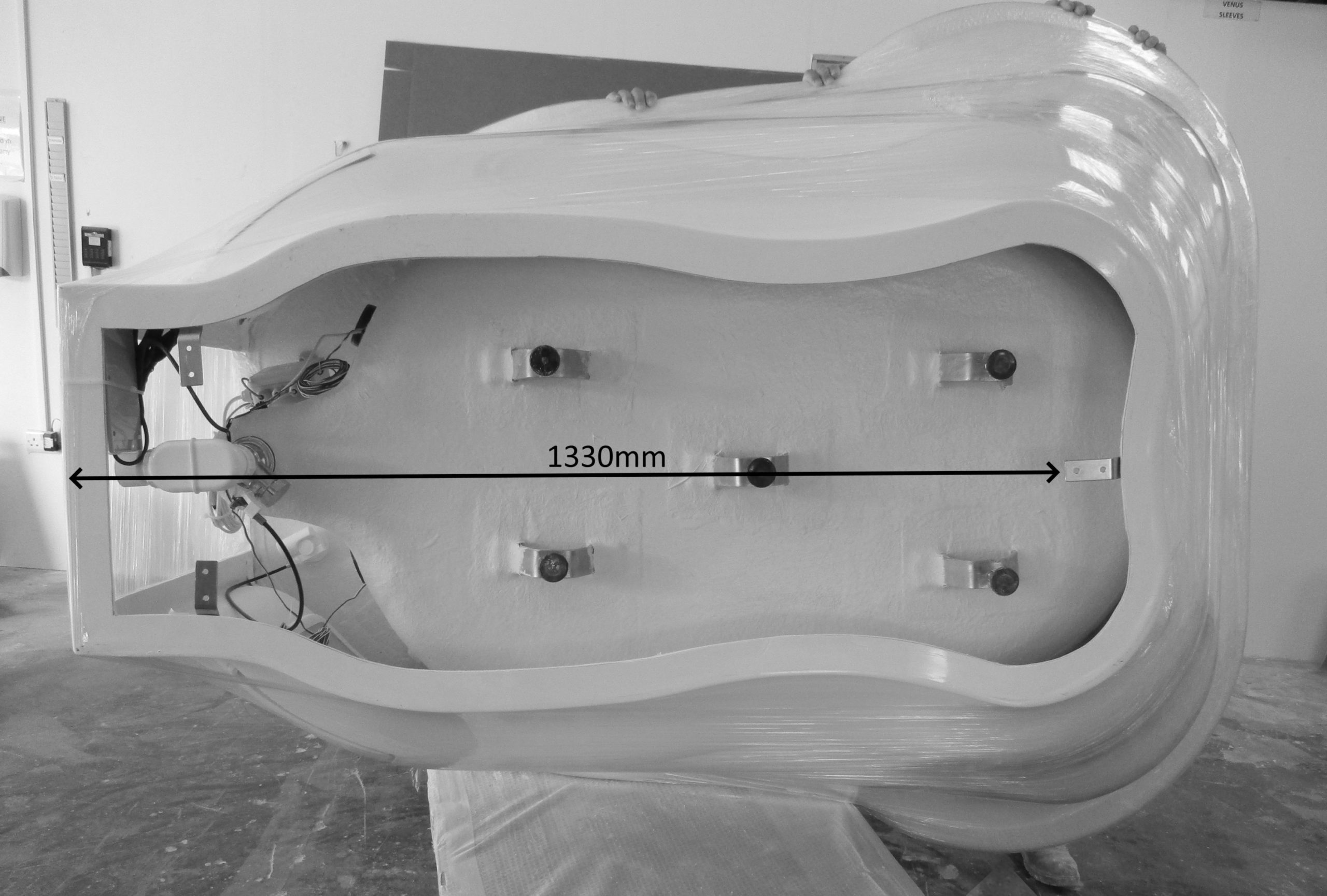
Front bracket right centre – Back bracket lower left and right
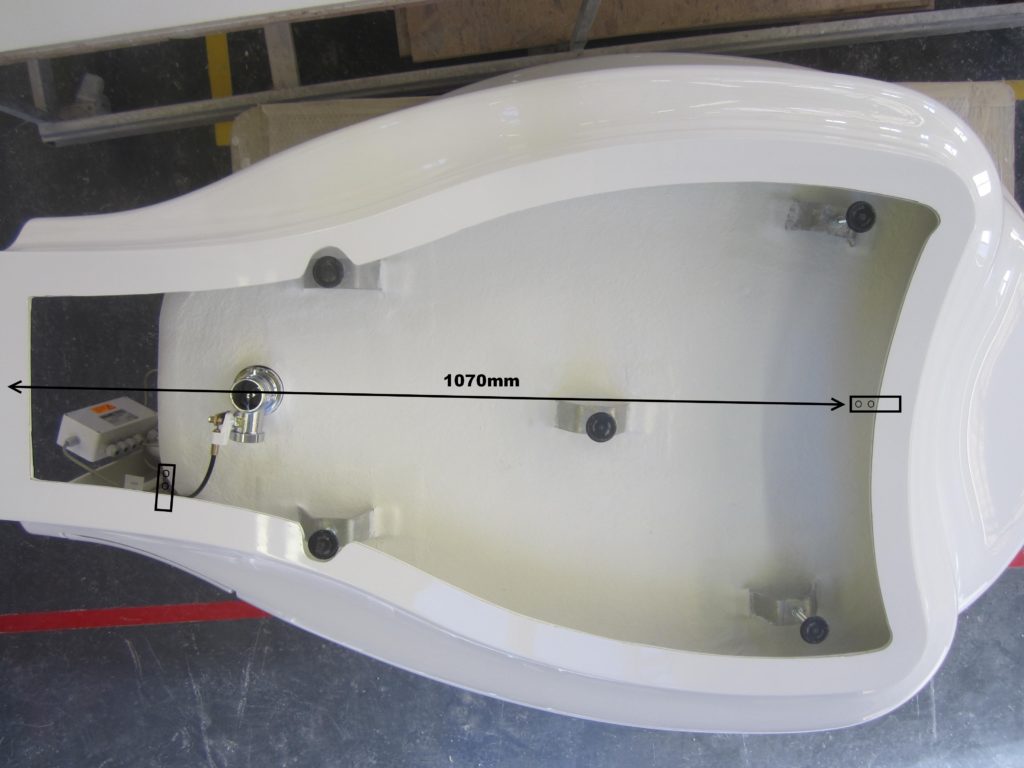
Step 2: Venus Birth Pool – front fixing bracket
Measure 1070 mm from the centre point on the wall and mark this as the point to locate the bracket so that the long flat piece is projecting away from the wall and raised short section faces forward into the room.
Fix the bracket to the floor using suitable hardware.
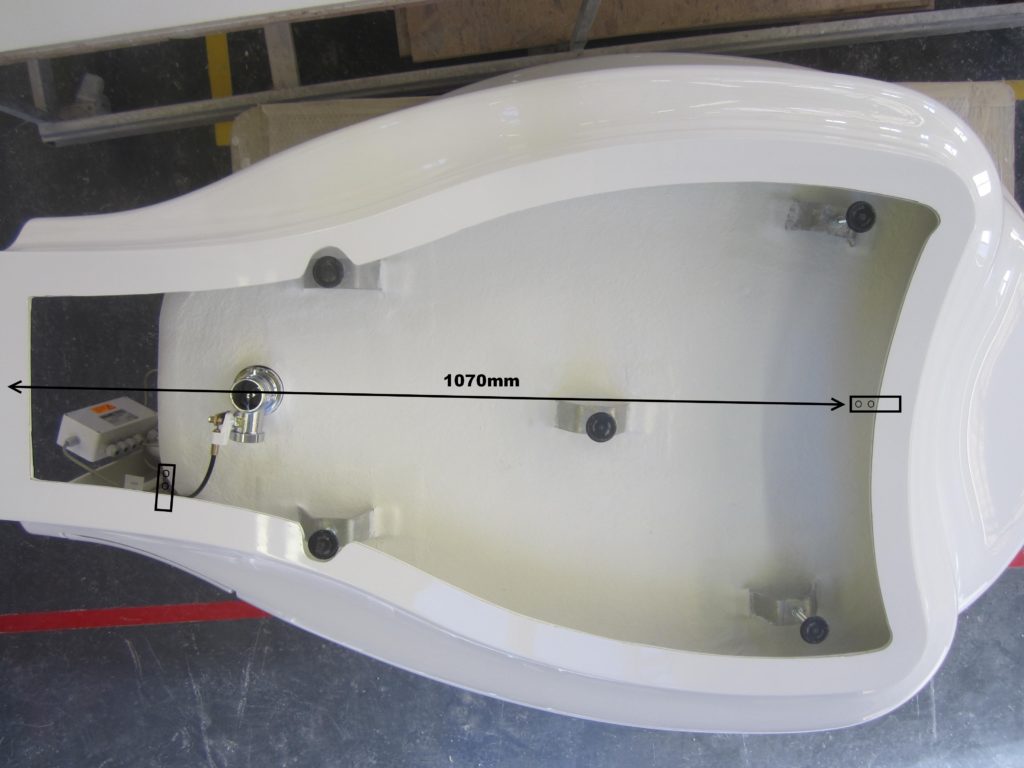
Front bracket right centre – Back bracket lower left
Step 2: Venus II Water Birth Pool
– front fixing bracket
Measure 1330 mm from the centre point on the wall and mark this as the point to locate the bracket so that the long flat piece is projecting away from the wall and the raised short section faces forward into the room.
Fix the bracket to the floor using suitable hardware.
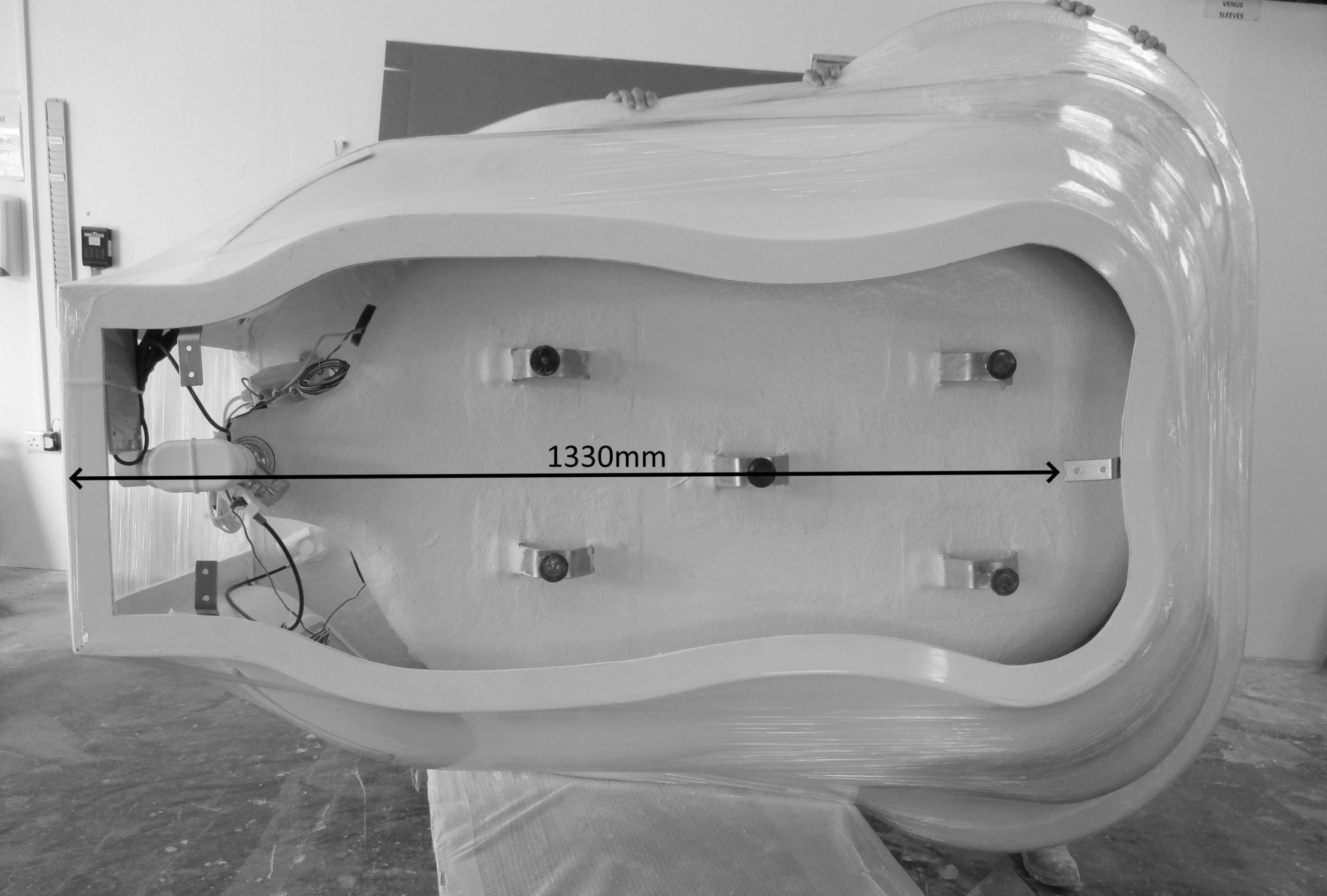
Front bracket right centre – Back bracket lower left and rightt
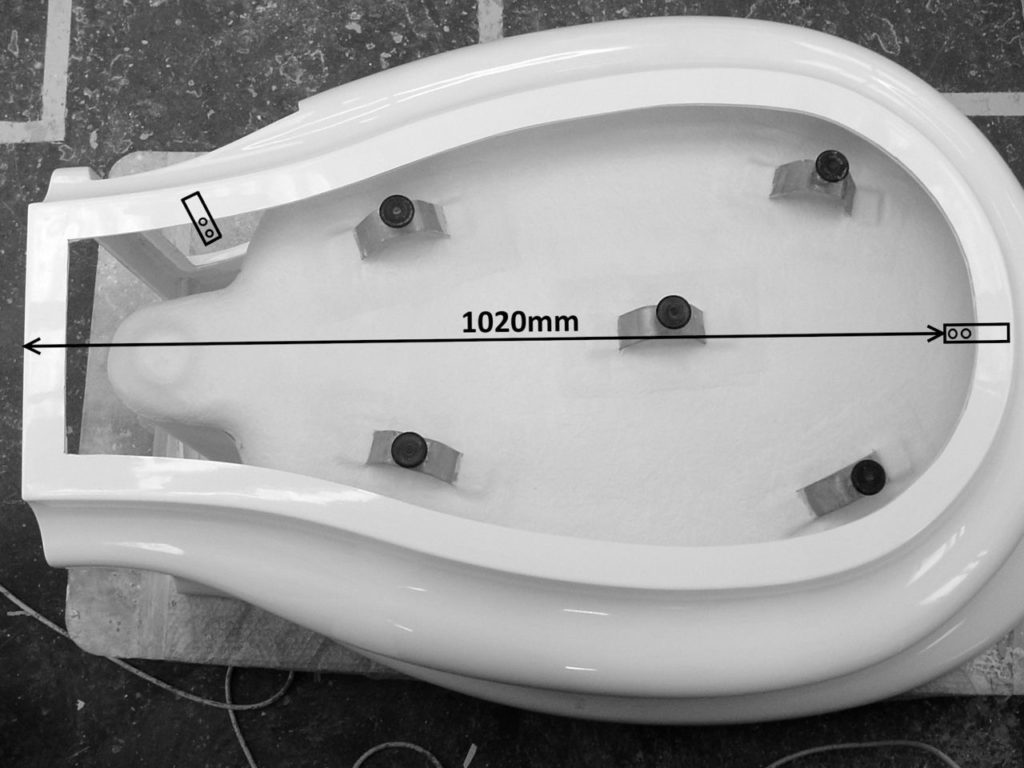
Step 2: Princess Birth Pool Pool – front fixing bracket
Measure 1020 mm from the centre point on the wall and mark this as the point to locate the bracket so that the long flat piece is projecting away from the wall and raised short section faces forward into the room.
Fix the bracket to the floor using suitable hardware.
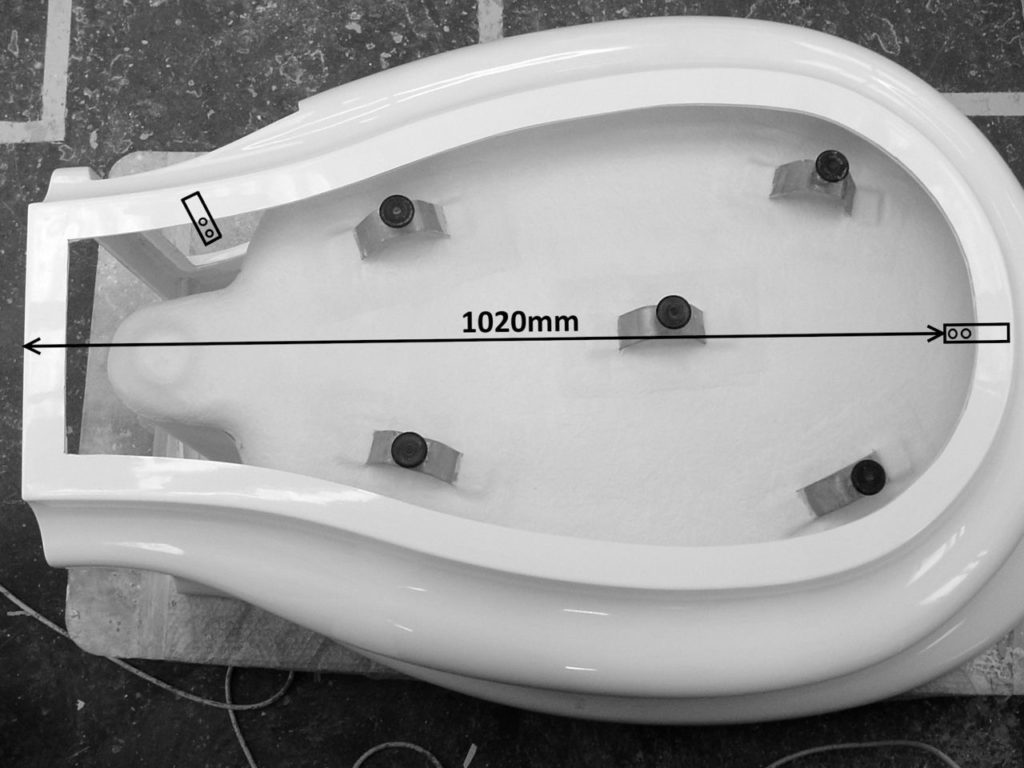
Front bracket right centre – Back bracket upper left
Step 3: All Models
Place the birth pool at least 60 mm away from the rear wall before moving it onto the bracket and flush against the wall.
Push the birth pool towards the wall so that the flange of the pool slides under the bracket.
This secures the front of the pool to the floor.
Step 4: All Models – back fixing bracket
The 2nd fixing bracket should be fixed in position on the bottom flange of the pool below the access panel as indicated in the images above.
You will see that a hole has been drilled in the flange. Line the bracket up with this hole. You can fix the pool to the floor with a raw plug and suitable hardware to guarantee that it is secure.
The long flat piece should be fixed to the floor with suitable hardware so that the short section is holding the flange securely to the floor.
Step 5: All Models
Seal the water birth pool to the floor and wall using a suitable sealant to prevent ingress of water and dirt.

Multi-Colour LED Lighting
Installation
Connect the light to a circuit breaker, then to the power supply.
The system should be protected by a 6 AMP RCD with 30 -32 MA Sensitivity.
The LED is transformed down to 12 volts and has a power rating of 2.5 watts.
A separate means of Isolation should be provided for future maintenance.
Operating voltage 220/230 volts – 50/60 hertz
Operating instructions
The system is operated by the control pad on the rim of the pool.
To activate the system press the button once.
The white light will come on.
To choose another colour continue to press the button and the system will cycle through the range of colours – light blue, blue, purple, magenta, red, pink, orange, yellow, apple green and green.
To turn the system off press and hold the button down for 2 seconds.
The light should be switched off when the pool is not in use.

Bluetooth Sound System
Connect the factory fitted bluetooth sound system to a circuit breaker and then to the power supply.
The system is always on standby waiting for users to pair and connect.
It’s operated directly from the users mobile phone or bluetooth enabled device and has no controls of its own.
N.B. If there is more than one birth pool with bluetooth sound being installed in the same unit you will need to fit a remote switch to enable the users to turn the system on and off.
This is to prevent people accidentally activating the system instead of the one in their room.
Transducer speaker
- Frequency Range 20Hz-20KHz.
- Maximum Power Output 50W at 4 Ohm.
Bluetooth Amplifier
- Transmission Range 5m to 10m.
- Maximum Power Output 2ch X 20W.
- Operating voltage 220/230 volts – 50/60 hertz
- Transformed Voltage 12 Volt DC / 3 amp.
- Waterproof Rating IP67.
Cleaning and Care:
Safety comes 1st!
Active Birth Pools are Rated No.1 for water safety and infection control standards.
This is because the material we use (Ficore) is 5 x harder than other materials and is immune to the effects of disinfection with 10,000ppm hypo-chlorite.
Seamless one-piece construction and the absence of surface mounted metal work deny micro-organisms the environment they need to propagate.
Active Birth Pools Cleaning and Disinfection Guidelines
This is a two-step procedure – first cleaning of the pool and surround, then disinfection of the pool and surround.
- Prior to emptying the pool remove debris and larger particles from the water with a sieve to prevent it from blocking or obstructing the outlet.
- Use the standard infection control precautions (plastic apron, disposable gloves and eye protection) when cleaning the pool. Ensure the area is well ventilated.
- Cleaning – use a non-abrasive detergeant with non-abrasive sponge or cloth to thoroughly clean the pool. Ensure the tap is cleaned first, so as not to transfer micro-organisms from the “dirty” pool area to the cleaner tap region. Rinse well with warm water.
- Disinfecting – use chlorclean or similar hypochlorite disinfectant following the directions on the packet for mixing the solution to the correct concentration for disinfecting the birth pool and surround. Do not use bleach as it is highly corrosive and could cause damage to the fittings.
- Apply the solution to the tap and spout prior to disinfecting the pool.
- There are 3 methods for disinfecting the pool that are commonly used in hospitals:
1) Fill the pool with cold water and add the requisite amount of disinfectant – leave for ten minutes.
The advantage of this method is that it is 100% effective but wasteful of water, time consuming and uses a large amount of disinfectant
2) Make up 2-3 litres of solution and pour it around the inside of the rim. Then use a new disposable mop or cloth to spread the disinfectant over the surface of the pool. Leave for ten minutes.
The advantage of this method is that it is economic in terms of time and cost but relies upon the person carrying out the task to ensure that 100% of the pools surface is disinfected.
3) Fill a spray bottle with disinfectant and thoroughly spray the surface of the pool and surround. Then use a new disposable mop or cloth to spread the disinfectant over the surface of the pool. Leave for ten minutes.
The advantage of this method is that it is economic in terms of time and cost but relies upon the person carrying out the task to ensure that 100% of the pools surface is disinfected
- Open the drain outlet and empty the pool of the disinfectant.
- Using cold water, rinse the tap then the pool to remove all traces of the disinfectant, to prevent any residue being left on the pool surface.
- Dry the entire surface of the pool using a new cloth or disposable mop head.
- Keep the drain outlet closed when not in use.
If you are duty flushing the taps with hot water/steam add a few inches of cold water to the pool first.
Damage resulting from higher water temperatures, steam cleaning or use of products not approved by Active Birth Pools will not be covered by our guarantee.
Protocols from hospitals using Active Birth Pools.
SaveSave
SaveSave
SaveSave
SaveSave
SaveSave