Water birth guidelines – Wirral Women’s and Children’s Hospital MLU

Guideline for the Management of Women Requesting Immersion in Water for Active Labour and/or Birth
Norfolk and Norwich University Hospitals
A clinical guideline recommended for use
Piscines de Naissance Active, créée en 1987, a joué un rôle de pionnière dans l’utilisation de l’eau pour le travail et l’accouchement.
Leurs valeurs et leur approche peuvent être pleinement comprises en examinant divers aspects de leurs opérations et de leurs produits.

Innovation et Esprit Pionnier:
Piscines de Naissance Active a contribué à pionnier l’utilisation de l’eau dans le travail et l’accouchement, travaillant en étroite collaboration avec les sages-femmes, les mères, les obstétriciens et les experts en contrôle des infections et en manutention manuelle.
Cette approche collaborative a conduit au développement de la première piscine d’accouchement en eau de qualité hospitalière spécialement conçue au monde, démontrant leur engagement envers l’innovation et l’amélioration des soins maternels.
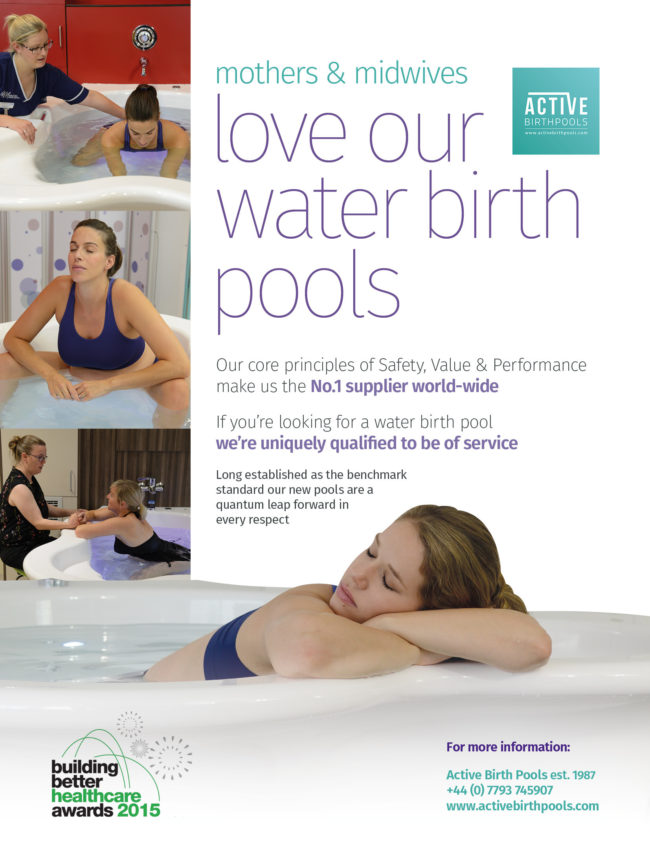
Seguridad, Valor y Rendimiento:
La empresa enfatiza estos principios fundamentales en sus productos.
Se centran en la producción de piscinas de parto que sean seguras, ofrezcan un gran valor y funcionen de manera excepcional.
Este enfoque se refleja en el uso de materiales especializados como el Ficore®, un material patentado conocido por su durabilidad, practicidad y características de seguridad.
Por ejemplo, las piscinas Ficore® retienen el calor de manera eficiente y son resistentes a las bacterias y a los desinfectantes fuertes, garantizando altos estándares de higiene.

Conception Ergonomique:
Piscines de Naissance Active utilise des principes de conception ergonomique basés sur des preuves et centrés sur l’utilisateur.
Leurs piscines sont conçues pour répondre aux besoins de confort des mères et des sages-femmes, avec des designs qui supportent diverses positions comme s’asseoir, s’agenouiller et se mettre en position accroupie.
Les larges rebords des piscines permettent aux sages-femmes de se reposer confortablement, semblable à s’asseoir à un bureau, ce qui témoigne de leur souci à la fois du confort des utilisateurs et de la praticité.
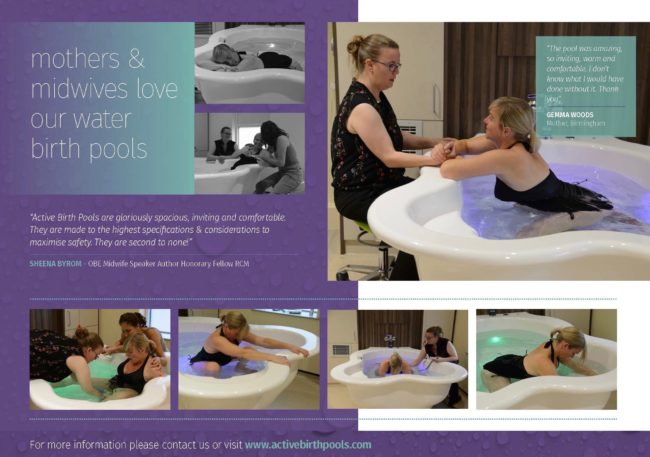
Avis des Clients et Recommandations:
La société accorde de l’importance aux commentaires des clients et a reçu de nombreux témoignages positifs de professionnels de la santé et de mères.
Ces témoignages mettent souvent en avant le confort, la facilité d’utilisation, la sécurité et la praticité des piscines, reflétant l’engagement de l’entreprise envers la qualité et la satisfaction des utilisateurs.

Qualité de Construction et Garantie:
Les piscines de Naissance Active sont fabriquées à la main sur commande en Angleterre par des artisans hautement qualifiés qui sont fiers de leur travail et dédiés à l’excellence.
Piscines de Naissance Active offre une garantie à vie sur ses piscines d’accouchement en eau, ce qui reflète leur engagement envers la qualité et la durabilité.
Cette garantie à vie est un témoignage de la confiance que l’entreprise place dans sa conception, ses matériaux et ses processus de fabrication.
Durabilité et Longévité:
Piscines de Naissance Active accorde de l’importance à la durabilité.
Leurs piscines ont une espérance de vie dépassant les 25 ans, ce qui en fait un choix durable par rapport à d’autres piscines d’accouchement ayant des durées de vie plus courtes.
Cette longévité offre non seulement un bon rapport qualité-prix, mais est également conforme aux principes de durabilité environnementale.

Portée et Expérience Mondiales:
Avec une histoire s’étendant sur plusieurs décennies, Piscines de Naissance Active a fourni des milliers de piscines d’accouchement en eau dans le monde entier.
Leur vaste expérience et leurs connaissances dans le domaine en ont fait un choix de premier plan pour les hôpitaux et les sages-femmes à l’échelle mondiale.
Cette portée mondiale souligne leur engagement à améliorer les soins maternels à l’échelle mondiale.
En résumé, les valeurs de Piscines de Naissance Active sont centrées sur l’innovation, la sécurité, la conception ergonomique, la satisfaction du client, la durabilité et une perspective mondiale pour améliorer les soins maternels.
Ces valeurs ont guidé leurs opérations et le développement de leurs produits, les positionnant comme un leader sur le marché des piscines d’accouchement en eau.
في الساحة المتطورة باستمرار لرعاية الأمومة، تسعى المستشفيات باستمرار إلى وسائل مبتكرة لتعزيز تجربة الولادة للأمهات المتوقعات. إحدى هذه الابتكارات التي تكتسب قوة هي دمج حمامات المياه خلال مرافق المستشفيات. بعيدًا عن أن تكون مجرد اتجاهٍ، تقدم حمامات المياه للولادة فوائد كثيرة لا تقتصر فقط على أولياء الأمور ولكن تساهم أيضًا في تحسين تجربة الولادة بشكل شامل وتعزيز الشعور بالتمكين. في هذا المقال، سنتناول الأسباب المقنعة التي يجب على المستشفيات أن تفكر في اعتناق هذا التوجه ودمج حمامات المياه في خدمات رعاية الأمومة الخاصة بها.

تخفيف الألم بشكل طبيعي:
لقد تم التعرف على الماء منذ فترة طويلة كمسكن طبيعي قوي. الانغماس في الماء الدافئ يمكن أن يخفف من شدة التقلصات ويوفر إحساسًا بعدم الوزن، مما يقلل من تأثير الجاذبية على الجسم. تقدم المستشفيات التي توفر حمامات المياه للولادة للأمهات خيار إدارة الألم البديل الذي يكمل الطرق التقليدية، مما يوفر نهجًا أكثر شخصنة للراحة خلال الولادة. أظهرت العديد من الدراسات فعالية الانغماس في الماء في تخفيف ألم الولادة. خلصت مراجعة نشرت في “مجلة التعليم الأمومي” (هاربر وآخرون، 2016) إلى أن الانغماس في الماء الدافئ أثناء الولادة يقلل بشكل كبير من تصور الألم، مما يوفر للأمهات المتوقعات خيارًا لتخفيف الألم غير دوائي ومستند إلى الأدلة. تشير الأبحاث المنشورة في “مجلة التمريض النسائي والتوليدي وحديثي الولادة” (ثويني وآخرون، 2019) إلى أن الانغماس في الماء أثناء الولادة يقلل من هرمونات التوتر، مما يعزز حالة أكثر استرخاءً للأم والطفل. ربط انخفاض مستويات هرمونات التوتر بتحسين الرفاهية الأمومية والنتائج المواتية للولادة، مما يدعم الحجة لحمامات المياه كنهج شامل لرعاية الأمومة.

تقليل التوتر والقلق:
يمكن أن يكون عملية الولادة مصدر قلق للعديد من الأمهات المتوقعات. تخلق حمامات المياه للولادة بيئة هادئة ومهدئة، تعزز الاسترخاء وتقلل من مستويات التوتر. تعزز الطفو في الماء إحساسًا بعدم الوزن، مما يسمح للأمهات بالحركة بحرية أكبر وتبني وضعيات مريحة، مما يسهم في تجربة ولادة إيجابية وممكنة بشكل أكبر. تشير الأبحاث المنشورة في “مجلة التمريض النسائي والتوليدي وحديثي الولادة” (ثويني وآخرون، 2019) إلى أن الانغماس في الماء أثناء الولادة يقلل من هرمونات التوتر، مما يعزز حالة أكثر استرخاءً للأم والطفل. رُبطت مستويات منخفضة لهرمونات التوتر بتحسين الرفاهية الأمومية والنتائج المواتية للولادة، مما يدعم الحجة لحمامات المياه كنهج شامل لرعاية الأمومة.

تسهيل الحركة والتوجيه:
توفر حمامات المياه للولادة بيئة تسهل الحركة والتوجيه خلال عملية الولادة. يسمح الطفو بزيادة القدرة على الحركة، مما يتيح للأمهات تغيير وضعياتهن بسهولة والعثور على أكثر وضع مريح للولادة. يمكن أن تعزز هذه المرونة تقدم عملية الولادة وتسهل عملية الولادة. أظهرت دراسة نشرت في “المجلة الأمريكية لطب النساء والتوليد” (زانيتي-دالينباخ وآخرون، 2007) أن الانغماس في الماء يعزز القدرة على الحركة لدى الأمهات خلال الولادة. يسمح طفو الماء بحركة وتوجيه أسهل، مما قد يقلل من مدة الولادة ويقلل من الحاجة إلى التدخلات. تؤكد هذه الأدلة على أهمية حمامات المياه في توفير بيئة تسهل التوجيه الأمثل لعملية الولادة.

تحسين الدورة الدموية:
الماء الدافئ في حمام الولادة يعزز تحسين الدورة الدموية، وهو ما يمكن أن يكون مفيدًا بشكل خاص خلال عملية الولادة. تساعد التداول المحسّن في التقليل من الانتفاخ وتعزيز تدفق الأكسجين، مما يسهم في رفاهية الأم والطفل على حد سواء. تعتبر المستشفيات التي تدمج حمامات المياه للولادة أولوية للجوانب الفسيولوجية للولادة، معززة بذلك بيئة ولادة أكثر صحة. لقد تم توثيق التأثير الإيجابي للانغماس في الماء الدافئ على الدورة الدموية بشكل جيد. أظهرت دراسة سيطرية عشوائية نشرت في “مجلة القابلات وصحة المرأة” (بيرنز وآخرون، 2012) أن الانغماس في الماء الدافئ يزيد من تدفق الدم في الأطراف وتأكسجها، مما يوفر فوائد فسيولوجية تسهم في الرفاه العام للأم والطفل.

تعزيز الرباط:
الإعداد الحميم والخاص لحمام الولادة يشجع على مشاركة الشريك ويعزز الرباط الأعمق بين الآباء والمولود الجديد. تجربة الولادة المشتركة في حمام الولادة يمكن أن تعزز الرابط العاطفي بين الشركاء، معززةً الشعور بالوحدة والمسؤولية المشتركة في استقبال أحدث أفراد العائلة. أجريت دراسة شاملة للميتا نشرت في “مجلة الولادة: قضايا الرعاية خلال فترة ما بعد الولادة” (نيكوديم وآخرون، 2016) لفحص النتائج النفسية للانغماس في الماء أثناء الولادة. أظهر التحليل وجود ترابط إيجابي بين تجارب الولادة في الماء وزيادة الرضا الأمومي والرباط مع المولود الجديد.

ختام:
المستشفيات التي تعتبر إدماج حمامات المياه للولادة أولوية تتماشى مع الأدلة التي تدعم الفوائد العاطفية لهذا النهج في الولادة. إدماج حمامات المياه في خدمات الرعاية بالمستشفى للأمومة يمثل خطوة تقدمية نحو توفير نهج أكثر شمولًا وتركيزًا على المريض في عملية الولادة. فوق الفوائد الجسدية، مثل تخفيف الألم الطبيعي وتحسين الدورة الدموية، تساهم حمامات المياه للولادة في تحسين تجربة عاطفية أكثر غنى للوالدين. مع سعي المستشفيات للأولوية لرفاهية وتفضيلات الأمهات المتوقعات، يظهر إدماج حمامات المياه كخيار مقنع، مستذكرًا الارتباط القديم بين الإنسانية وضمان الماء المهدئ خلال معجزة الولادة. إدماج حمامات المياه في خدمات الرعاية بالمستشفى للأمومة ليس مجرد خطوة تقدمية؛ بل هو قفزة مدعومة علميا نحو توفير تجارب الولادة القائمة على الأدلة ومحورة حول المريض. تعزيز فوائد الانغماس في الماء خلال الولادة من خلال العديد من الدراسات يعزز الفكرة بأنه يجب على المستشفيات أن تعتبر حمامات المياه للولادة ليست فاخرة بل عنصرًا حيويًا في تعزيز بيئة ولادة آمنة ومريحة وقائمة على الأدلة. إن جمود الأدلة يدعم بقوة إدماج حمامات المياه كقوة محولة في رعاية الأمومة الحديثة.
Nel sempre mutevole panorama dell’assistenza alla maternità, gli ospedali sono costantemente alla ricerca di modi innovativi per migliorare l’esperienza del parto per le future mamme.
Una tale innovazione che sta guadagnando slancio è l’integrazione delle piscine per il parto in acqua all’interno delle strutture ospedaliere.
Lontane dall’essere una semplice tendenza, le piscine per il parto in acqua offrono una miriade di vantaggi che non solo prioritizzano il benessere sia della madre che del bambino, ma contribuiscono anche a un’esperienza di parto più olistica e potenziante.
In questo articolo, approfondiamo le ragioni convincenti per cui gli ospedali dovrebbero considerare di abbracciare la marea e integrare le piscine per il parto in acqua nei loro servizi di assistenza alla maternità.

Sollievo Naturale dal Dolore:
L’acqua è da lungo tempo riconosciuta come un potente alleviatore naturale del dolore.
Immergersi in acqua calda può alleviare l’intensità delle contrazioni e fornire una sensazione di leggerezza, riducendo l’impatto della gravità sul corpo.
Gli ospedali che offrono piscine per il parto in acqua forniscono alle madri un’opzione alternativa di gestione del dolore che integra i metodi tradizionali, offrendo un approccio più personalizzato al comfort durante il travaglio.
Numerosi studi hanno dimostrato l’efficacia dell’immersione in acqua nel alleviare il dolore del travaglio.
Una revisione pubblicata nel “Journal of Perinatal Education” (Harper et al., 2016) ha concluso che l’immersione in acqua calda durante il travaglio riduce significativamente la percezione del dolore, offrendo alle future mamme un’opzione di sollievo dal dolore non farmacologica e basata su prove scientifiche.
La ricerca pubblicata nel “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) suggerisce che l’immersione in acqua durante il travaglio riduca gli ormoni dello stress, promuovendo uno stato più rilassato sia per la madre che per il bambino.
Livelli inferiori di ormoni dello stress sono stati associati a un miglioramento del benessere materno e a risultati di parto favorevoli, supportando l’argomento a favore delle piscine per il parto in acqua come approccio olistico all’assistenza alla maternità.

Riduzione dello Stress e dell’Ansia:
Il processo di parto può essere una fonte di ansia per molte future mamme.
Le piscine per il parto in acqua creano un ambiente tranquillo e rilassante, favoriscono il relax e riducono i livelli di stress. La galleggiabilità dell’acqua promuove una sensazione di leggerezza, consentendo alle madri di muoversi più liberamente e adottare posizioni confortevoli, contribuendo a un’esperienza di parto più positiva e potenziante.
La ricerca pubblicata nel “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) suggerisce che l’immersione in acqua durante il travaglio riduca gli ormoni dello stress, promuovendo uno stato più rilassato sia per la madre che per il bambino.
Livelli inferiori di ormoni dello stress sono stati associati a un miglioramento del benessere materno e a risultati di parto favorevoli, supportando l’argomento a favore delle piscine per il parto in acqua come approccio olistico all’assistenza alla maternità.

Facilitazione del Movimento e Posizionamento:
Le piscine per il parto in acqua forniscono un ambiente favorevole al movimento e al posizionamento durante il travaglio.
La galleggiabilità consente una maggiore mobilità, permettendo alle madri di cambiare posizioni facilmente e trovare la postura più confortevole per il parto. Questa flessibilità può migliorare il progresso del travaglio e facilitare un processo di parto più scorrevole.
Uno studio pubblicato nell'”American Journal of Obstetrics & Gynecology” (Zanetti-Daellenbach et al., 2007) ha dimostrato che l’immersione in acqua potenzia la mobilità materna durante il travaglio.
La galleggiabilità dell’acqua consente un movimento e un posizionamento più facili, abbreviando potenzialmente la durata del travaglio e riducendo la necessità di interventi.
Queste evidenze sottolineano l’importanza delle piscine per il parto in acqua nel fornire un ambiente favorevole per posizioni ottimali di parto.

Miglioramento della Circolazione Sanguigna:
L’acqua calda in una piscina per il parto favorisce un miglioramento della circolazione sanguigna, particolarmente benefico durante il travaglio.
Una circolazione potenziata aiuta a ridurre il gonfiore e favorisce il flusso di ossigeno, contribuendo al benessere sia della madre che del bambino.
Gli ospedali che incorporano piscine per il parto in acqua prioritizzano gli aspetti fisiologici del parto, promuovendo un ambiente di parto più sano. L’impatto positivo dell’immersione in acqua calda sulla circolazione sanguigna è ben documentato.
Uno studio controllato randomizzato pubblicato nel “Journal of Midwifery & Women’s Health” (Burns et al., 2012) ha rivelato che l’immersione in acqua calda aumenta il flusso sanguigno periferico e l’ossigenazione, fornendo benefici fisiologici che contribuiscono al benessere complessivo sia della madre che del bambino.

Potenziamento del Legame:
L’ambiente intimo e privato di una piscina per il parto in acqua favorisce il coinvolgimento del partner e promuove una connessione più profonda tra i genitori e il neonato.
L’esperienza condivisa del travaglio e del parto in una piscina per il parto in acqua può rafforzare il legame emotivo tra i partner, promuovendo un senso di unità e responsabilità condivisa nell’accogliere il nuovo membro della famiglia.
Un’ampia meta-analisi pubblicata su “Birth: Issues in Perinatal Care” (Nikodem et al., 2016) ha esaminato gli esiti psicologici dell’immersione in acqua durante il travaglio.
L’analisi ha riscontrato una correlazione positiva tra le esperienze di parto in acqua e un aumento della soddisfazione materna e del legame con il neonato.

Conclusioni:
Gli ospedali che danno priorità all’inclusione delle piscine per il parto in acqua si allineano alle prove che sostengono i benefici emotivi di questo approccio al parto.
L’inclusione delle piscine per il parto in acqua nei servizi di assistenza alla maternità degli ospedali rappresenta un passo progressivo verso un approccio più completo e centrato sul paziente al parto.
Oltre ai benefici fisici, come il sollievo naturale dal dolore e il miglioramento della circolazione, le piscine per il parto in acqua contribuiscono a un’esperienza emotivamente arricchente sia per i genitori.
Mentre gli ospedali si sforzano di dare priorità al benessere e alle preferenze delle future mamme, l’integrazione delle piscine per il parto in acqua emerge come una scelta convincente, riecheggiando l’antico legame tra l’umanità e l’abbraccio lenitivo dell’acqua durante il miracolo del parto.
Incorporare le piscine per il parto in acqua nei servizi di assistenza alla maternità degli ospedali non è solo un passo progressivo; è un balzo scientificamente supportato verso la fornitura di esperienze di parto basate su prove e centrate sul paziente.
La moltitudine di studi a sostegno dei benefici dell’immersione in acqua durante il travaglio rafforza l’idea che gli ospedali dovrebbero considerare le piscine per il parto in acqua non come un lusso, ma come un elemento cruciale nel favorire un ambiente di parto sicuro, confortevole e basato su prove scientifiche.
La marea di prove supporta in modo schiacciante l’integrazione delle piscine per il parto in acqua come una forza trasformatrice nell’assistenza moderna alla maternità.
L’apice del design e dello sviluppo delle piscine per il parto
Il video “Libertà di Movimento” raggiunge 12.000.000 di visualizzazioni su YouTube!
Perché le piscine per il parto attivo sono la scelta numero 1 a livello mondiale
In der sich ständig entwickelnden Landschaft der Geburtshilfe suchen Krankenhäuser kontinuierlich nach innovativen Möglichkeiten, um die Geburtserfahrung für werdende Mütter zu verbessern.
Eine solche Innovation, die an Dynamik gewinnt, ist die Integration von Gebärwannen in Krankenhauseinrichtungen.
Weit davon entfernt, nur ein Trend zu sein, bieten Gebärwannen eine Vielzahl von Vorteilen, die nicht nur das Wohlbefinden von Mutter und Kind priorisieren, sondern auch zu einer ganzheitlicheren und stärkenden Geburtserfahrung beitragen.
In diesem Artikel gehen wir auf die überzeugenden Gründe ein, warum Krankenhäuser in Betracht ziehen sollten, die Flut zu umarmen und Gebärwannen in ihre Geburtshilfeleistungen zu integrieren.

Natürliche Schmerzlinderung:
Wasser wird schon lange als leistungsstarkes natürliches Schmerzmittel anerkannt.
Das Eintauchen in warmes Wasser kann die Intensität von Wehen lindern und ein Gefühl der Schwerelosigkeit vermitteln, wodurch der Einfluss der Schwerkraft auf den Körper verringert wird.
Krankenhäuser, die Gebärwannen anbieten, bieten Müttern eine alternative Schmerzmanagementoption, die traditionelle Methoden ergänzt und einen persönlicheren Ansatz zum Wohlbefinden während der Geburt bietet. Zahlreiche Studien haben die Wirksamkeit der Wasserimmersion zur Linderung von Geburtsschmerzen nachgewiesen.
Eine Überprüfung, die im “Journal of Perinatal Education” (Harper et al., 2016) veröffentlicht wurde, kam zu dem Schluss, dass das Eintauchen in warmes Wasser während der Geburt die Schmerzwahrnehmung signifikant reduziert und werdenden Müttern eine nicht-pharmakologische und evidenzbasierte Schmerzlinderungsoption bietet.
Forschung, die im “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) veröffentlicht wurde, legt nahe, dass Wasserimmersion während der Geburt Stresshormone reduziert und einen entspannteren Zustand sowohl für die Mutter als auch das Baby fördert.
Niedrigere Stresshormonspiegel wurden mit verbessertem mütterlichem Wohlbefinden und günstigen Geburtsergebnissen in Verbindung gebracht, was die Argumentation für Gebärwannen als ganzheitlichen Ansatz zur Geburtshilfe unterstützt.

Reduzierter Stress und Angst:
Der Geburtsprozess kann für viele werdende Mütter eine Quelle von Angst sein. Gebärwannen schaffen eine ruhige und beruhigende Umgebung, fördern die Entspannung und reduzieren den Stress.
Die Auftriebskraft des Wassers fördert ein Gefühl der Schwerelosigkeit, das es Müttern ermöglicht, sich freier zu bewegen und bequeme Positionen einzunehmen, was zu einer positiveren und stärkenden Geburtserfahrung beiträgt.
Forschung, die im “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) veröffentlicht wurde, legt nahe, dass Wasserimmersion während der Geburt Stresshormone reduziert und einen entspannteren Zustand sowohl für die Mutter als auch das Baby fördert.
Niedrigere Stresshormonspiegel wurden mit verbessertem mütterlichem Wohlbefinden und günstigen Geburtsergebnissen in Verbindung gebracht, was die Argumentation für Gebärwannen als ganzheitlichen Ansatz zur Geburtshilfe unterstützt..

Förderung von Bewegung und Positionierung:
Gebärwannen bieten eine Umgebung, die förderlich für Bewegung und Positionierung während der Geburt ist. Die Auftriebskraft ermöglicht eine erhöhte Mobilität, wodurch Mütter leicht die Position wechseln und die bequemste Haltung für die Entbindung finden können.
Diese Flexibilität kann den Fortschritt der Geburt verbessern und einen reibungsloseren Geburtsprozess erleichtern. Eine im “American Journal of Obstetrics & Gynecology” (Zanetti-Daellenbach et al., 2007) veröffentlichte Studie ergab, dass das Eintauchen in Wasser die mütterliche Mobilität während der Geburt verbessert.
Die Auftriebskraft des Wassers ermöglicht eine einfachere Bewegung und Positionierung, was möglicherweise die Dauer der Geburt verkürzt und den Bedarf an Interventionen verringert.
Diese Evidenz unterstreicht die Bedeutung von Gebärwannen, um eine förderliche Umgebung für optimale Geburtspositionen zu bieten.

Verbesserte Blutzirkulation:
Das warme Wasser in einer Gebärwanne fördert eine verbesserte Blutzirkulation, was während der Geburt besonders vorteilhaft sein kann.
Die verbesserte Zirkulation hilft dabei, Schwellungen zu reduzieren und den Sauerstofffluss zu fördern, was zum Wohlbefinden von Mutter und Baby beiträgt.
Krankenhäuser, die Gebärwannen integrieren, priorisieren die physiologischen Aspekte der Geburt und fördern eine gesündere Geburtsumgebung.
Die positive Auswirkung der warmen Wasserimmersion auf die Blutzirkulation ist gut dokumentiert.
Eine randomisierte kontrollierte Studie, die im “Journal of Midwifery & Women’s Health” (Burns et al., 2012) veröffentlicht wurde, zeigte, dass das Eintauchen in warmes Wasser den peripheren Blutfluss und die Sauerstoffversorgung erhöht und physiologische Vorteile bietet, die zum allgemeinen Wohlbefinden von Mutter und Baby beitragen.

Vertiefte Bindung:
Die intime und private Umgebung einer Gebärwanne ermutigt zur Beteiligung des Partners und fördert eine tiefere Verbindung zwischen den Eltern und dem Neugeborenen.
Die gemeinsame Erfahrung von Geburt und Entbindung in einer Gebärwanne kann die emotionale Bindung zwischen Partnern stärken und ein Gefühl der Einheit und gemeinsamen Verantwortung bei der Begrüßung des neuesten Familienmitglieds fördern.
Eine umfassende Metaanalyse, die im “Birth: Issues in Perinatal Care” (Nikodem et al., 2016) veröffentlicht wurde, untersuchte die psychologischen Ergebnisse der Wasserimmersion während der Geburt.
Die Analyse ergab eine positive Korrelation zwischen Erfahrungen mit Wasserentbindung und gesteigerter mütterlicher Zufriedenheit und Bindung zum Neugeborenen.

Fazit:
Krankenhäuser, die die Integration von Gebärwannen priorisieren, stehen im Einklang mit Evidenz, die die emotionalen Vorteile dieses Geburtsansatzes unterstützt.
Die Integration von Gebärwannen in die Geburtshilfeleistungen von Krankenhäusern stellt einen progressiven Schritt dar, um einen umfassenderen und patientenzentrierten Ansatz zur Geburt zu bieten.
Über die physischen Vorteile hinaus, wie natürliche Schmerzlinderung und verbesserte Zirkulation, tragen Gebärwannen zu einer emotional bereichernden Erfahrung für beide Eltern bei.
Da Krankenhäuser danach streben, das Wohlbefinden und die Vorlieben werdender Mütter zu priorisieren, zeigt sich die Integration von Gebärwannen als überzeugende Wahl und spiegelt die jahrhundertealte Verbindung zwischen der Menschheit und der beruhigenden Umarmung von Wasser während des Wunders der Geburt wider.
Die Integration von Gebärwannen in die Geburtshilfeleistungen von Krankenhäusern ist nicht nur ein progressiver Schritt; es handelt sich um einen wissenschaftlich unterstützten Schritt, um evidenzbasierte, patientenzentrierte Geburtserlebnisse zu ermöglichen.
Die Vielzahl von Studien, die die Vorteile der Wasserimmersion während der Geburt unterstützen, unterstreicht die Auffassung, dass Krankenhäuser Gebärwannen nicht als Luxus, sondern als entscheidendes Element betrachten sollten, um eine sichere, komfortable und evidenzbasierte Geburtsumgebung zu fördern.
Die Flut an Beweisen unterstützt überwältigend die Integration von Gebärwannen als transformative Kraft in der modernen Geburtshilfe.
Der Höhepunkt der Entwicklung und des Designs von Wassergeburtsbecken
Freiheit der Bewegung” erreicht 12.000.000 Aufrufe auf YouTube!
Dans le paysage en constante évolution des soins maternels, les hôpitaux cherchent continuellement des moyens novateurs pour améliorer l’expérience de l’accouchement pour les futures mamans.
Une innovation qui gagne du terrain est l’intégration de piscines d’accouchement aquatiques dans les installations hospitalières.
Bien loin d’être une simple tendance, les piscines d’accouchement aquatiques offrent une myriade d’avantages qui mettent non seulement l’accent sur le bien-être de la mère et de l’enfant, mais contribuent également à une expérience d’accouchement plus holistique et émancipatrice.
Dans cet article, nous explorons les raisons convaincantes pour lesquelles les hôpitaux devraient envisager d’adopter la marée et d’intégrer des piscines d’accouchement aquatiques dans leurs services de soins maternels.

Soulagement naturel de la douleur:
L’eau est depuis longtemps reconnue comme un puissant analgésique naturel.
S’immerger dans l’eau chaude peut atténuer l’intensité des contractions et procurer une sensation d’apesanteur, réduisant l’impact de la gravité sur le corps.
Les hôpitaux proposant des piscines d’accouchement aquatiques offrent aux mères une option de gestion de la douleur alternative qui complète les méthodes traditionnelles, offrant une approche plus personnalisée du confort pendant le travail.
De nombreuses études ont démontré l’efficacité de l’immersion dans l’eau pour soulager la douleur du travail.
Une revue publiée dans le “Journal of Perinatal Education” (Harper et al., 2016) a conclu que l’immersion dans l’eau chaude pendant le travail réduit significativement la perception de la douleur, offrant aux futures mamans une option de soulagement de la douleur non pharmacologique et fondée sur des preuves.
Des recherches publiées dans le “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) suggèrent que l’immersion dans l’eau pendant le travail réduit les hormones du stress, favorisant un état plus détendu tant pour la mère que pour le bébé.
Des niveaux réduits d’hormones de stress ont été associés à une amélioration du bien-être maternel et à des résultats favorables à la naissance, étayant l’argument en faveur des piscines d’accouchement aquatiques en tant qu’approche holistique des soins maternels.

Réduction du stress et de l’anxiété :
Le processus d’accouchement peut être une source d’anxiété pour de nombreuses futures mamans.
Les piscines d’accouchement aquatiques créent un environnement tranquille et apaisant, favorisant la relaxation et réduisant les niveaux de stress.
La flottabilité de l’eau favorise une sensation d’apesanteur, permettant aux mères de se déplacer plus librement et d’adopter des positions confortables, contribuant à une expérience d’accouchement plus positive et émancipatrice.
Des recherches publiées dans le “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) suggèrent que l’immersion dans l’eau pendant le travail réduit les hormones du stress, favorisant un état plus détendu tant pour la mère que pour le bébé.
Des niveaux réduits d’hormones de stress ont été associés à une amélioration du bien-être maternel et à des résultats favorables à la naissance, étayant l’argument en faveur des piscines d’accouchement aquatiques en tant qu’approche holistique des soins maternels.

Facilitation du mouvement et du positionnement:
Les piscines d’accouchement aquatiques offrent un environnement propice au mouvement et au positionnement pendant le travail.
La flottabilité permet une mobilité accrue, permettant aux mères de changer facilement de position et de trouver la posture la plus confortable pour l’accouchement.
Cette flexibilité peut améliorer le déroulement du travail et faciliter un processus d’accouchement plus fluide.
Une étude publiée dans l'”American Journal of Obstetrics & Gynecology” (Zanetti-Daellenbach et al., 2007) a révélé que l’immersion dans l’eau améliore la mobilité maternelle pendant le travail.
La flottabilité de l’eau permet un mouvement et un positionnement plus faciles, raccourcissant potentiellement la durée du travail et réduisant la nécessité d’interventions.
Cette preuve souligne l’importance des piscines d’accouchement aquatiques en fournissant un environnement propice aux positions d’accouchement optimale

Amélioration de la circulation sanguine:
L’eau chaude dans une piscine d’accouchement favorise une meilleure circulation sanguine, ce qui peut être particulièrement bénéfique pendant le travail.
Une circulation améliorée aide à réduire le gonflement et à favoriser le flux d’oxygène, contribuant au bien-être tant de la mère que du bébé. Les hôpitaux qui intègrent des piscines d’accouchement aquatiques accordent la priorité aux aspects physiologiques de l’accouchement, favorisant un environnement d’accouchement plus sain.
L’impact positif de l’immersion dans l’eau chaude sur la circulation sanguine a été largement documenté.
Un essai contrôlé randomisé publié dans le “Journal of Midwifery & Women’s Health” (Burns et al., 2012) a révélé que l’immersion dans l’eau chaude augmente le flux sanguin périphérique et l’oxygénation, offrant des avantages physiologiques qui contribuent au bien-être global tant de la mère que du bébé.

Renforcement des liens :
Le cadre intime et privé d’une piscine d’accouchement dans l’eau encourage la participation du partenaire et favorise une connexion plus profonde entre les parents et le nouveau-né.
L’expérience partagée du travail et de l’accouchement dans une piscine d’accouchement dans l’eau peut renforcer le lien émotionnel entre les partenaires, favorisant un sentiment d’unité et de responsabilité partagée dans l’accueil du nouveau membre de la famille.
Une méta-analyse complète publiée dans “Birth: Issues in Perinatal Care” (Nikodem et al., 2016) a examiné les résultats psychologiques de l’immersion dans l’eau pendant le travail.
L’analyse a trouvé une corrélation positive entre les expériences d’accouchement dans l’eau et une satisfaction maternelle accrue ainsi qu’un renforcement des liens avec le nouveau-né.

Conclusion:
Les hôpitaux qui donnent la priorité à l’inclusion de piscines d’accouchement dans l’eau s’alignent sur des preuves soutenant les avantages émotionnels de cette approche de l’accouchement.
L’inclusion de piscines d’accouchement dans l’eau dans les services de maternité des hôpitaux représente une avancée vers une approche plus globale et centrée sur le patient de l’accouchement.
Au-delà des avantages physiques, tels que le soulagement naturel de la douleur et l’amélioration de la circulation, les piscines d’accouchement dans l’eau contribuent à une expérience plus enrichissante émotionnellement pour les parents.
Alors que les hôpitaux s’efforcent de donner la priorité au bien-être et aux préférences des futures mères, l’intégration de piscines d’accouchement dans l’eau se présente comme un choix convaincant, résonnant avec la connexion séculaire entre l’humanité et l’étreinte apaisante de l’eau lors du miracle de l’accouchement.
L’intégration de piscines d’accouchement dans l’eau dans les services de maternité des hôpitaux n’est pas simplement une avancée, c’est un saut soutenu scientifiquement vers la fourniture d’expériences d’accouchement fondées sur des preuves et centrées sur le patient.
La multitude d’études soutenant les avantages de l’immersion dans l’eau pendant le travail renforce l’idée que les hôpitaux devraient considérer les piscines d’accouchement dans l’eau non pas comme un luxe, mais comme un élément crucial pour favoriser un environnement d’accouchement sûr, confortable et fondé sur des preuves.
Liberté de Mouvement” atteint 12 000 000 de vues sur YouTube !
Le summum de la conception et du développement de la baignoire de naissance
Enquanto a importância de projetar piscinas de parto aquático para as mães é evidente, a importância de projetar para as parteiras é fundamental.
As mães podem usar as piscinas algumas vezes, mas as parteiras as utilizam continuamente.
As parteiras nos dizem que nossas piscinas de parto aquático são as mais confortáveis e fáceis de usar.

Elas apreciam o fato de estarem protegidas do risco de lesões e se beneficiarem do nível incomparável de conforto e apoio que recebem.
As parteiras relatam melhores resultados e dizem que nossas piscinas são fabulosas e um prazer de usar.
E é por isso que, dado uma escolha, as parteiras preferem as Piscinas de Parto Ativo.

Em 1995, trabalhamos com a Ergonomista de Serviço de Saúde Sue Hignett e as parteiras do Nottingham City Hospital para analisar maneiras de melhorar o design de nossas piscinas de parto aquático.
Descobrimos que nossas piscinas poderiam ser tornadas dramaticamente mais seguras, confortáveis e fáceis de usar.
Os resultados estão apresentados neste artigo, “Melhorando o Design de Piscinas de Parto”, publicado no Chartered Institute of Ergonomics and Human Factors.

Se você observar nossas piscinas de parto desde o início da década de 1990 (acima), notará imediatamente os painéis de saia verticais e as bordas estreitas.
O problema é que as parteiras não podem sentar confortavelmente, próximas à mãe.
A piscina se torna um obstáculo entre a mãe e a parteira.
As parteiras são forçadas a sentar longe da piscina com as pernas abertas para dar espaço e depois se inclinam para frente.
Isso cria a dinâmica física ideal que causa dor lombar (uma reclamação comum das parteiras que assistem a partos na água).
Para piorar, as bordas estreitas não são confortáveis para descansar, pois a pressão é concentrada em uma pequena área do antebraço.

As fotos acima mostram como, com nossas piscinas de parto aquático, as parteiras podem se sentar próximas à mãe com total conforto.
O painel de saia côncavo é contornado para a forma da piscina, dando às parteiras bastante espaço sob a borda para suas pernas.
Elas se sentam com os braços apoiados na borda em formato de touro, extra larga, assim como você faria em uma mesa.
Além disso, a borda não é obstruída com torneiras e conexões, o que permite que as parteiras se movam facilmente ao redor da circunferência da piscina conforme necessário.

Os parceiros desempenham um papel importante no trabalho de parto e no parto.
Nossas piscinas permitem que os casais fiquem próximos e íntimos sem a necessidade de o parceiro entrar na água.
Esse suporte (tanto físico quanto psicológico) pode fazer toda a diferença para ajudar as mães a terem uma experiência de trabalho de parto fisiológico e um parto natural.

As Piscinas de Parto Ativo oferecem às parteiras opções seguras e práticas para facilitar evacuações de emergência – com ou sem um guindaste.
A monitorização pode ser facilmente realizada sem que a mãe precise sair da piscina.
As mães podem entrar facilmente em nossas piscinas sem subir em grandes e volumosas unidades de degraus, o que coloca tanto as mães quanto as parteiras em risco.
Por que as Piscinas de Parto Ativas são a escolha número 1 em todo o mundo
O pináculo do design e desenvolvimento das piscinas de nascimento
O vídeo “Liberdade de Movimento” alcança 12.000.000 de visualizações no YouTube!
Questo breve video con oltre 12.000.000 di visualizzazioni mostra che le madri hanno spazio per muoversi liberamente nelle posizioni naturali del travaglio e del parto.
Come instintivamente si relazionano alle nostre piscine per il parto in acqua e si muovono naturalmente per trovare le posizioni più comode e benefiche.
La libertà di movimento combinata agli effetti rilassanti dell’acqua calda potenzia il rilascio di ossitocina, aumentando significativamente la probabilità che le madri vivano un travaglio fisiologico e un parto naturale.
L’apice del design e dello sviluppo delle piscine per il parto
هذا الفيديو القصير الذي حصل على أكثر من 12,000,000 مشاهدة يظهر أن لديهن الأمهات مساحة للتحرك بحرية في الوضعيات الطبيعية للولادة والإنجاب.
كيف ترتبط نفسيًا بحمامات الولادة في الماء لدينا وتتحرك بشكل طبيعي للعثور على أكثر الوضعيات راحةً وفائدةً.
الحرية في الحركة مجتمعة مع التأثيرات الاسترخائية للماء الدافئ تعزز من إفراز الأوكسيتوسين مما يزيد بشكل كبير من احتمالية أن تعيش الأمهات عملية الولادة الفسيولوجية والولادة الطبيعية بشكل كبير.
Este curto vídeo, com mais de 12.000.000 de visualizações, mostra que as mães têm espaço para se mover livremente nas posturas naturais do trabalho de parto e do parto.
Como elas se relacionam instintivamente com as nossas piscinas de parto na água e se movem naturalmente para encontrar as posições mais confortáveis e benéficas.
A liberdade de movimento combinada com os efeitos relaxantes da água morna aumenta a liberação de ocitocina, o que aumenta significativamente a probabilidade de as mães experimentarem o trabalho de parto fisiológico e o parto natural.
Por que as Piscinas de Parto Ativas são a escolha número 1 em todo o mundo
O pináculo do design e desenvolvimento das piscinas de nascimento
Os juízes dos prestigiados Prêmios Europeus de Design concederam o primeiro prêmio à Piscina de Parto na Água Active II/360 na Categoria de Segurança em Saúde.
O Prêmio Europeu de Design de Produto (ePDA) é um evento global de ponta dedicado a elevar e promover a arte do Design de Produto.
O Prêmio Europeu de Design de Produto™ reconhece os esforços de talentosos designers de produtos internacionais que visam melhorar nosso cotidiano com suas criações práticas e bem elaboradas.
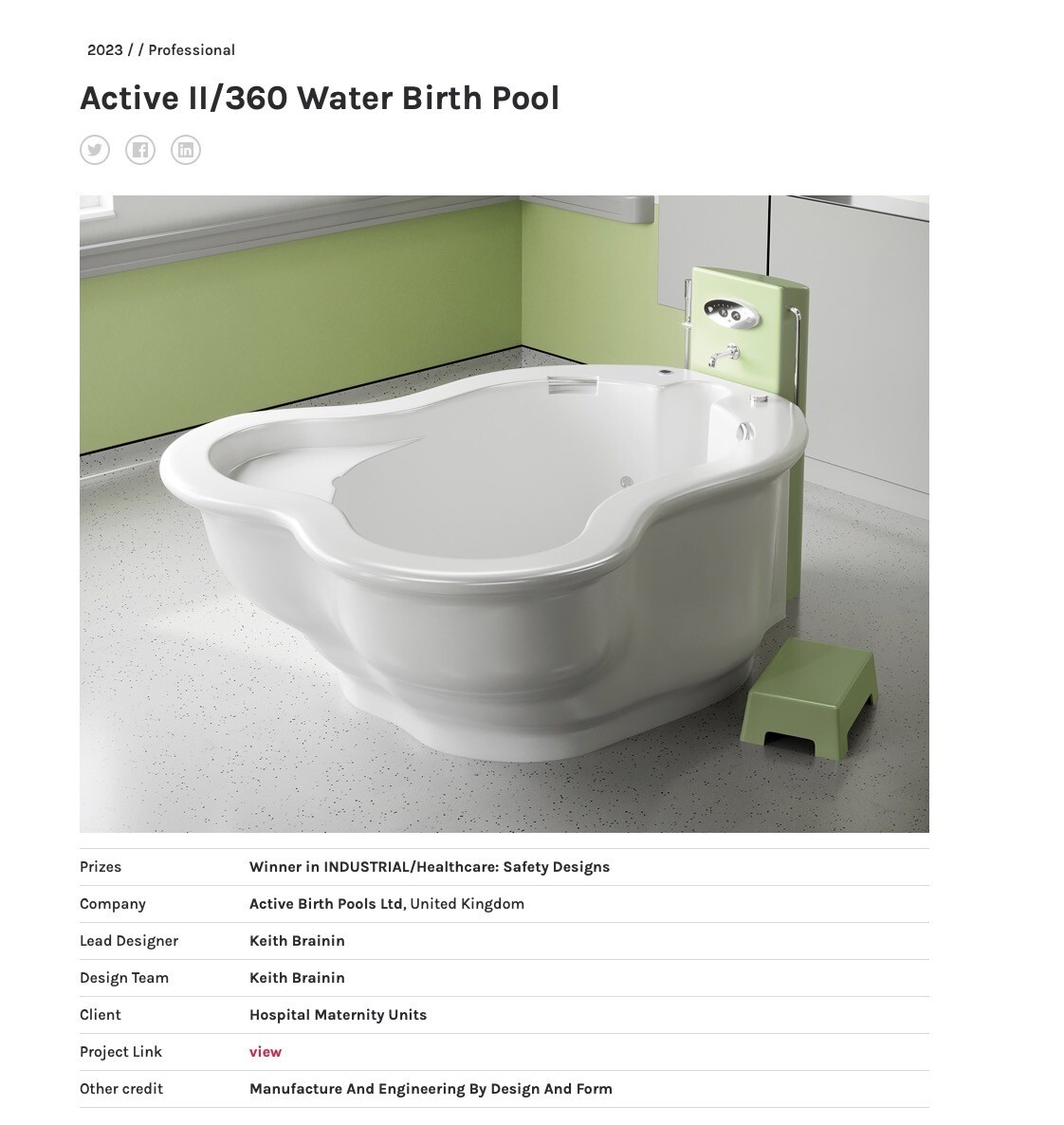
Apresentando a Banheira de Parto Aquático Active II/360 com Coluna de Água Personalizada: Um Ponto Alto da Inovação em Cuidados Maternos
Active Birth Pools oferece a Banheira de Parto Aquático Active II/360 com Coluna de Água Personalizada, uma solução sofisticada sob medida para instalações de saúde que buscam fornecer cuidados maternos exemplares.
Esta combinação avançada integra uma banheira de parto aquático de última geração com uma coluna de água funcional e estilosa, simbolizando o que há de mais moderno em inovação de design e tecnologia de materiais para o setor de cuidados maternos.
Desenvolvimento Avançado para as Necessidades da Saúde Moderna
A Banheira de Parto Aquático Active II/360, um produto da Active Birth Pools, é projetada para atender às demandas em evolução dos cuidados maternos contemporâneos.
Emparelhada com a Coluna de Água Personalizada, este sistema é o resultado de extensa pesquisa e colaboração com profissionais de saúde.
O foco tem sido criar uma solução que ofereça funcionalidade, segurança e conforto superiores, abordando também as necessidades práticas de prestadores de cuidados de saúde e mães.

Design Ergonômico para uma Experiência Aprimorada
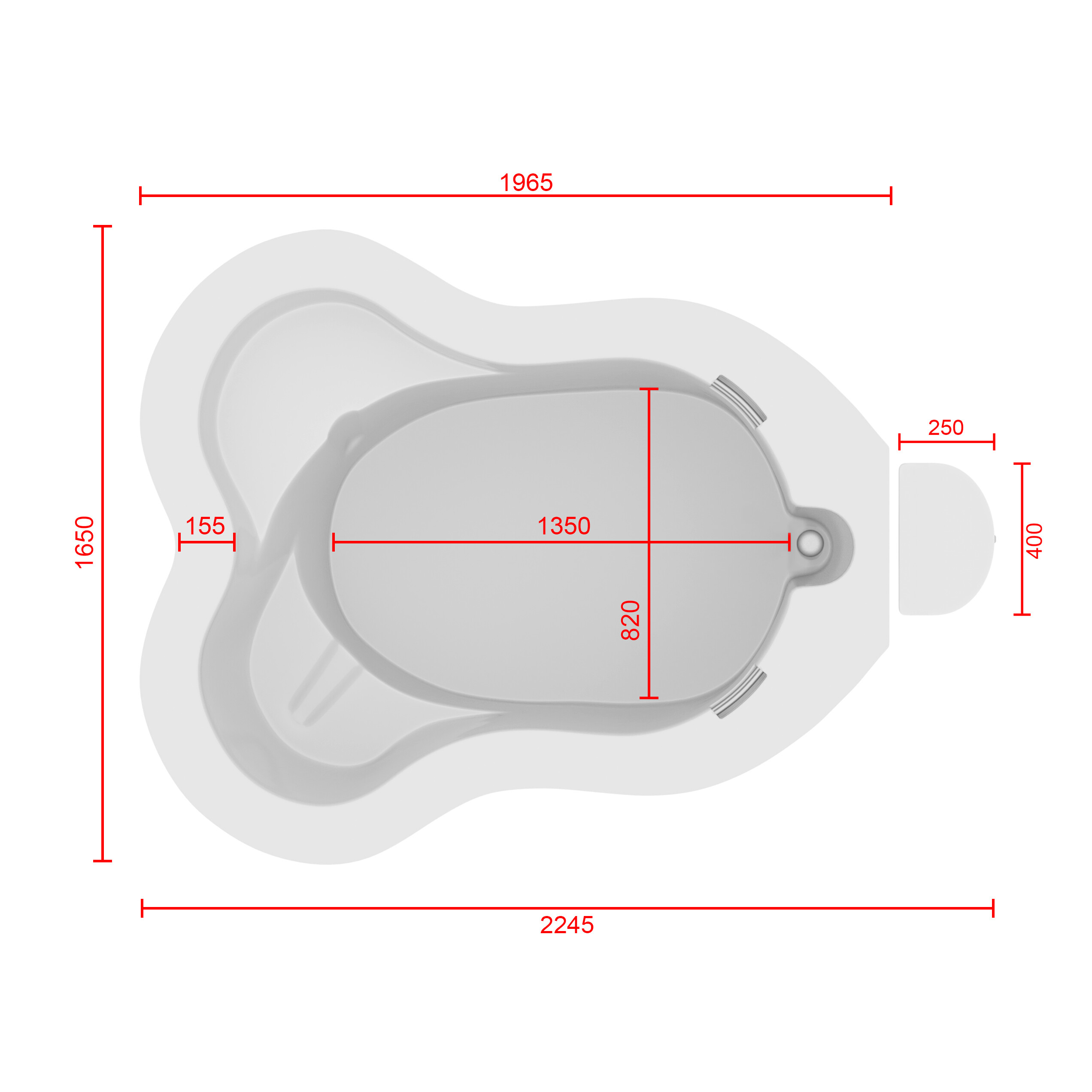
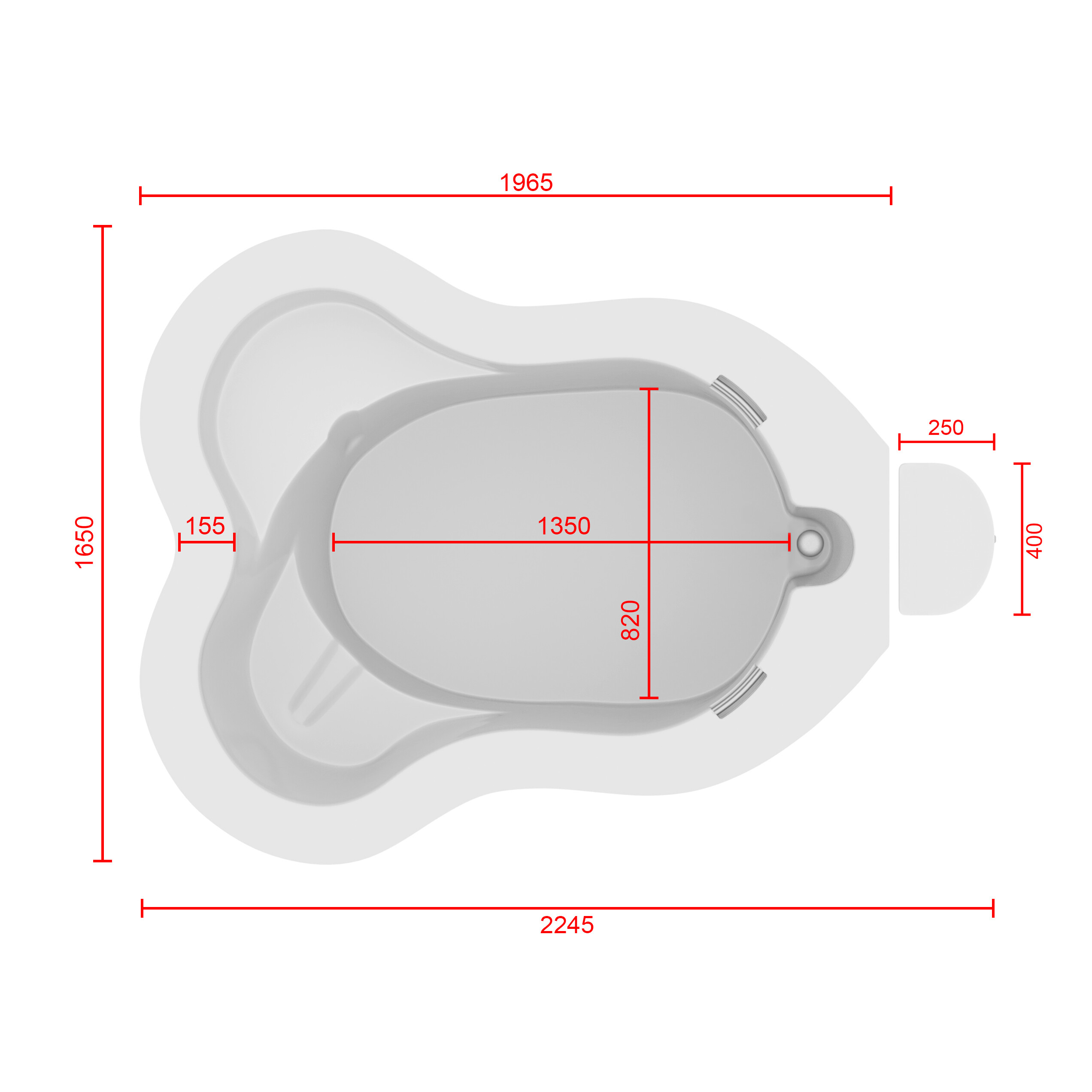
A Banheira de Parto Aquático Active II/360 é projetada com ênfase na excelência ergonômica e eficiência espacial.
A forma de buraco de fechadura da piscina não é apenas visualmente atraente, mas também proporciona benefícios funcionais, suportando uma variedade de posições e movimentos de parto.
A piscina inclui alças de mão embutidas e uma borda em forma de nariz de touro para suporte e segurança adicionais.
A Coluna de Água Personalizada é integrada de forma harmoniosa, oferecendo uma solução elegante para as necessárias instalações hidráulicas e acessórios, aprimorando assim a utilidade e estética da piscina.

Qualidade Superior de Material
Construída a partir de Ficore®, um material composto proprietário exclusivo da Active Birth Pools, a Active II/360 oferece durabilidade, higiene e segurança excepcionais.
A superfície do material é altamente polida e ultra-lisa, menos propensa a escorregadios, crucial para garantir segurança.
A Coluna de Água, feita do mesmo material de alta qualidade, complementa o design da piscina e mantém os altos padrões de higiene exigidos em ambientes de saúde.

Recursos Centrados no Usuário
A Banheira de Parto Aquático Active II/360 com Coluna de Água inclui um assento de apoio ao trabalho de parto, facilitando o posicionamento e conforto ótimos para a mãe, e um assento de segurança no nível da borda para monitoramento e evacuações de emergência.
O design da piscina permite movimento livre, essencial para o uso eficaz da imersão em água durante o trabalho de parto.
A Coluna de Água adiciona funcionalidade como uma estrutura de apoio estável e uma plataforma utilitária prática.

Melhorias Tecnológicas Integradas
A piscina está equipada com Iluminação LED Multicolorida e Sistemas de Som Bluetooth, possibilitando a criação de um ambiente personalizado e tranquilizador.
Esses recursos são fundamentais para estabelecer uma atmosfera de apoio propícia ao parto natural.

Sustentabilidade e Benefícios Econômicos
O design durável da Banheira de Parto Aquático Active II/360 com Coluna de Água Personalizada a torna uma escolha sustentável e economicamente viável para instalações de saúde.
Seu desempenho de longo prazo e a redução da necessidade de substituições frequentes a tornam um investimento eficiente, alinhando-se com os objetivos econômicos e ambientais das instituições de saúde modernas.

Adoção Global e Reconhecimento
A Banheira de Parto Aquático Active II/360 com Coluna de Água Personalizada tem sido reconhecida globalmente por sua abordagem inovadora aos cuidados maternos.
Sua adoção por instalações de saúde em todo o mundo é um testemunho de sua eficácia, confiabilidade e compromisso em avançar nas práticas de parto na água.
Em conclusão, a Banheira de Parto Aquático Active II/360 com Coluna de Água Personalizada da Active Birth Pools representa uma combinação harmoniosa de design avançado, tecnologia de material superior e integração ponderada de recursos centrados no usuário.
Ela se destaca como uma escolha estratégica e inovadora para instalações de saúde que buscam oferecer uma experiência superior de cuidados maternos, proporcionando conforto, segurança e eficiência em um pacote abrangente e elegante.
Active II/360 Water Birth Pool – Ficha Técnica


Posicione o cursor sobre o modelo abaixo para mover a imagem ao redor.
Para ver como a Banheira de Parto Aquático Active II/360 ficaria em sua sala de parto, clique no banner abaixo com seu telefone ou tablet.
Quando se trata da criação e cuidado de instalações de parto na água, nada é mais importante do que a Saúde e Segurança.
Micro-organismos se proliferam livremente em ambientes úmidos e quentes e devem ser impedidos de se propagar.
O potencial das piscinas de parto na água em serem tanto um habitat quanto um meio de entrega para bactérias nocivas como Pseudomonas e Legionella é bem conhecido.
Nós entendemos completamente isso e projetamos nossas piscinas de parto na água para otimizar a segurança, negar risco e proporcionar ambientes de nascimento mais seguros.

Construção única e contínua em Ficore combinada com o mínimo de acessórios resulta em piscinas de parto na água de higiene e segurança da água sem paralelo.
Piscinas de Parto Ativo são fabricadas a partir de um material proprietário com qualidades únicas chamado composto Ficore®.
Ficore tem um grau muito mais alto de resistência, durabilidade e resistência a bactérias quando comparado a fibra de vidro ou acrílico.
Construção única e contínua em Ficore® melhora a higiene ao negar às bactérias o ambiente para crescer.
A superfície ultra-dura torna nossas piscinas de parto na água mais fáceis de limpar e mais resistentes a bactérias

Com as Regulações do Departamento de Saúde como diretriz, utilizamos design inteligente e uma série de inovações para negar risco e maximizar a segurança da água.
Além das vantagens que Ficore oferece às nossas piscinas do ponto de vista material, precisamos olhar para as vantagens que ele proporciona do ponto de vista de engenharia e fabricação.
As propriedades únicas do Ficore nos permitem projetar nossas piscinas com formas orgânicas e fluidas que melhoram a higiene ao facilitar uma limpeza mais eficaz.
O acabamento super liso e os contornos fluidos otimizam o escoamento e eliminam “armadilhas de sujeira”.

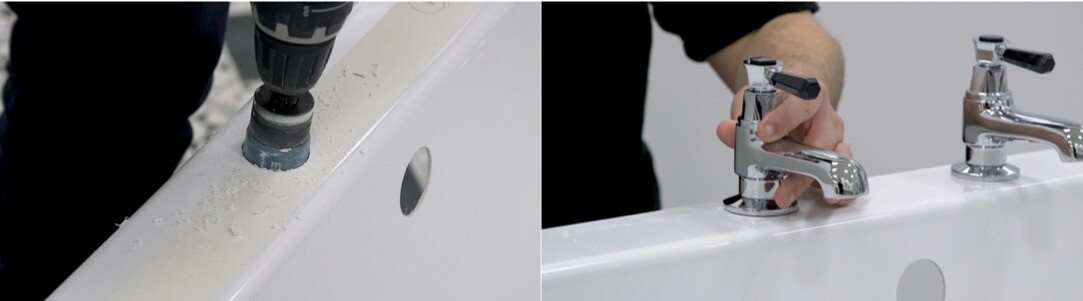
Piscinas de Parto Ativo: Acessórios e Instalações

Pegas de mão
Nossas pegas de mão em aço inoxidável, fornecidas pelo renomado fabricante de metal Samuel Heath, são coladas diretamente na piscina
Elas não são montadas na superfície como em outras piscinas de parto.
A barra é solidamente selada no tecido da piscina com Ficore.
Não há lacunas – não há movimento.
Isso torna impossível a penetração de umidade e a proliferação de bactérias

Sistema de Drenagem
Nosso sistema de drenagem é projetado e fabricado segundo os mais altos padrões.
Foi objeto de interesse de várias investigações por especialistas em controle de infecções, todos eles que voltaram para nos dar sua aprovação.
O resíduo fica em um recesso e é duplamente selado com silicone para um selo resistente à água e bactérias.
Os acessórios de aço inoxidável são feitos de latão sólido e não serão danificados pelo uso de cloridratos e outros desinfetantes.
O plugue pode ser retirado e embebido em hipoclorito entre os nascimentos.
A roda de controle montada na borda pode ser facilmente removida para limpeza.

Iluminação LED Subaquática Multicolorida
O encaixe de luz interna encaixa-se rente à parede lateral, possui uma moldura de aço inoxidável e é selado com silicone.
Devido ao fato de que os acessórios são estanques e montados verticalmente, a água não pode penetrar ou acumular.
O interruptor de controle na borda também é estanque e totalmente selado.

Torneiras e Chuveiros
Não fornecemos torneiras, mas recomendamos misturadores termostáticos de banho ou banho/chuveiro de 3/4″ como o Rada T3.
As torneiras nunca são montadas na borda, mas na parede ou coluna de água, como mostrado acima.
Os bicos devem estar a 25 cm acima da borda para evitar contato com a água da piscina e proteger a mãe de bater a cabeça.
Chuveiros de mão são muito úteis para limpar a piscina, mas devem ser destacáveis para que possam ser removidos enquanto a piscina está em uso.
A Coluna de Água
Piscinas de parto na água independentes estão se tornando cada vez mais populares.
Essas instalações normalmente apresentam riscos significativos de segurança da água e higiene, pois a encanamento e as instalações montadas na borda proporcionam o ambiente perfeito para a proliferação de micro-organismos.
Para instalações montadas na parede, as torneiras termostáticas, bico, chuveiro de mão e corrimão são fixados em um Painel IPS de acordo com as regulamentações do departamento de saúde.

Para piscinas de parto independentes, uma solução precisava ser encontrada.
Para resolver esse problema, desenvolvemos a Coluna de Água – um conceito de design sob medida que separa a encanamento da piscina para otimizar a higiene e a segurança da água e fornecer suporte crucial para mães e parteiras.
Seu design ergonômico elegante e altamente utilitário complementa a aparência e a usabilidade de nossas piscinas.
Instalações e Recursos Inseguros Comumente Encontrados em Piscinas de Parto na Água
Por estarem montados na piscina, próximos à água, o potencial de contaminação de instalações e acessórios montados na piscina por bactérias e infecção cruzada é muito aumentado.
Este banho de hidromassagem mostra claramente um grande número de instalações e sistemas inseguros, conforme aplicado a piscinas de parto na água. Observe o ralo de transbordamento, sistema de recirculação de água, torneira de pescoço de cisne, chuveiro integral, encanamento e controles montados na borda

Existem outros fabricantes que produzem piscinas de parto na água seguras, mas muitas piscinas de parto na água são equipadas com recursos que inicialmente podem parecer seguros ou até uma vantagem, mas na realidade apresentam riscos ou violam regulamentações.
Essas piscinas de parto na água (principalmente produzidas na Europa) são superdimensionadas e equipadas com uma profusão de acessórios e recursos que colocam mães e parteiras em risco.
Observe: as imagens de acessórios e recursos mostrados nesta seção são para fins ilustrativos e não mostram piscinas de parto reais.
Torneiras e Bicos Montados na Borda
Torneiras, bicos e chuveiros montados na borda são um dos maiores riscos de Saúde e Segurança
Esses acessórios apresentam um sério risco de controle de infecção, pois o espaço entre a superfície da piscina e o acessório é um terreno adequado para a proliferação de bactérias.
Lembre-se – as bactérias são microscópicas – mesmo que o acessório pareça nivelado com a superfície da piscina, há espaço para os micro-organismos se estabelecerem.
O risco de as bactérias se propagarem na umidade entre a placa e a borda é inaceitável.
Há também um risco de que as torneiras montadas na borda possam ser contaminadas com água da piscina e fluir de volta para a torneira.
Há o potencial de contaminação reversa da torneira, com colonização bacteriana no sistema em contravenção às regulamentações de encaixe de água
Torneiras e bicos para piscinas de parto na água devem ser montados na parede a 25 cm acima da piscina e equipados com proteção contra refluxo.
Há também um risco significativo de que as mães possam se machucar seriamente batendo a cabeça nessas torneiras.
Torneiras de Pescoço de Cisne
Torneiras de pescoço de cisne são frequentemente vistas montadas nas bordas das piscinas de parto na água. Embora atraentes, esse tipo de torneira representa um risco significativo de controle de infecção.
Torneiras de pescoço de cisne retêm volumes maiores de água, que então estagnam, e a HFN 30 e o HPSC recomendam que torneiras de pescoço de cisne não sejam usadas.
Isso ocorre porque elas não se esvaziam após o uso e podem estar propensas ao bioincrustamento microbiano com microrganismos, incluindo Legionella e P. aeruginosa, este último associado a uma torneira de pescoço de cisne durante o surto neonatal na Irlanda do Norte (HPSC, 2015).


Alças de Mão Montadas na Superfície (internas e montadas na borda)
Alças de mão montadas na superfície representam um sério risco de controle de infecção e manuseio manual.
Algumas piscinas de parto na água apresentam alças de mão montadas na superfície, semelhantes às mostradas acima.
Há um grande potencial para que as bactérias se estabeleçam entre o acessório e a piscina, tornando esses acessórios um risco inaceitável de controle de infecção.
O risco de infecção cruzada aumenta drasticamente com a presença de elementos metálicos montados na superfície, que entram em contato direto com a água enquanto a mãe utiliza a piscina.
Do ponto de vista do manuseio manual, essas alças de mão são perigosas, pois formam um obstáculo no qual as mães podem se machucar e interferem na movimentação ao redor da piscina.
Drenos de Transbordamento
Drenos de transbordamento abrigam bactérias e podem servir como conduto para infecções cruzadas.
As regulamentações são muito claras quanto a esse ponto.
Drenos de transbordamento não devem ser instalados em piscinas de parto na água, pois constituem um risco constante de controle de infecção.
Sistemas de Recirculação de Água
Sistemas de recirculação ou sistemas bombeados com jatos, como hidromassagens e jacuzzis, apresentam as condições ideais para o crescimento de micro-organismos.
Sistemas de água como esses representam os mais altos níveis de risco, pois produzem aerossóis.
Aerossóis são gerados quando a superfície da água é perturbada – por exemplo, com gotas de água caindo, respingos ou bolhas quebrando na superfície.
Uma vez introduzidos nesses sistemas, Legionella e Pseudomonas prosperam e podem se tornar aerosolizados e, em seguida, inalados.
Sistemas de Encanamento Integral
Sistemas de encanamento como esses utilizam tubulações flexíveis e não flexíveis, drenos de transbordamento, chuveiros portáteis, bombas, mangueiras, aquecedores, acessórios montados na superfície e filtros.
Esses sistemas são impossíveis de limpar, desinfetar ou monitorar e, portanto, representam um risco extremamente alto de controle de infecção.
Água estagnada dentro do sistema é um ambiente ideal para a proliferação de bactérias.
As regulamentações do Reino Unido afirmam que piscinas de parto na água devem ser abastecidas com torneiras de mistura termostática montadas na parede e conectadas diretamente à rede de água do hospital.

Chuveiros Portáteis
Chuveiros portáteis apresentam um risco significativo de controle de infecções.
Se o chuveiro cair na piscina, ele pode estar contaminado com bactérias que podem se reproduzir e serem transmitidas na próxima vez que o chuveiro for usado.
As regulamentações do Departamento de Saúde estipulam claramente que chuveiros portáteis e misturadores de banheira/chuveiro não devem ser instalados para uso em piscinas para parto na água, pois apresentam um risco de Categoria 5 para o abastecimento de água da rede pública.
Observação: Existem sistemas disponíveis que permitem que você desconecte a mangueira e a cabeça do chuveiro da torneira. Esses são permitidos desde que os acessórios do chuveiro sejam desconectados quando a piscina estiver em uso e só sejam usados posteriormente para a limpeza.
Sistemas de Aquecimento Bombeados
Sistemas de aquecimento para piscinas de parto na água não são necessários e apresentam riscos inaceitáveis de controle de infecções.
A água é bombeada através de um trocador de calor e depois volta para a piscina, criando o ambiente ideal para a reprodução de bactérias.
Esses sistemas representam um dos maiores riscos de controle de infecções e não devem ser utilizados.
Filtros de Bactérias e Sistemas de Desinfecção
Algumas piscinas para parto na água estão equipadas com esses dispositivos na tentativa de mitigar o risco de infecção e infestação por bactérias inerentes aos sistemas hidráulicos embutidos.
Filtros de bactérias e sistemas de desinfecção não podem ser considerados confiáveis e não garantirão padrões adequados de higiene.

Portas
Não há motivo para uma piscina de parto na água ter uma porta e muitos motivos pelos quais elas não deveriam ter.
As portas são erroneamente usadas por duas razões:
– Para facilitar evacuações de emergência
– Para ajudar as mães a entrar e sair da piscina
As portas apresentam um risco extremamente alto de infecção e devem ser proibidas de serem usadas em piscinas de parto na água apenas por esse motivo.
A vedação da porta (geralmente de espuma ou material emborrachado) é o local perfeito para a proliferação de bactérias.
Do ponto de vista do manuseio manual, as portas não são práticas ou adequadas para o propósito. Elas realmente complicam evacuações de emergência e colocam mães e parteiras em risco.
Wenn Sie nach einem Wassergebärbecken für Ihre Entbindungsstation suchen, können wir Ihnen unsere einzigartige Expertise anbieten
Wir haben wesentlich dazu beigetragen, den Weg für den Einsatz von Wasser bei Wehen und Entbindungen zu bahnen. Es war der Entwurf unserer Wassergebärbecken, der diese Revolution in der Geburtshilfe möglich gemacht hat
Wir liefern seit 1987 Gebärbecken an Hunderte Krankenhäuser in aller Welt und arbeiten eng mit unseren Kunden und mit technischen Experten zusammen, um unsere Produkte weiterzuentwickeln und zu verbessern

Dadurch verfügen wir über eine einzigartige Erfahrung in der Entwicklung und Herstellung von Gebärbecken, die sich durch außergewöhnlichen Nutzwert und unübertroffene Qualität auszeichnen
Seit langem setzen unsere Produkte den Maßstab für die gesamte Branche. Unsere neue Produktpalette an Gebärbecken stellt nun in jeder Hinsicht einen weiteren Quantensprung dar
Wir verbinden unsere reiche Erfahrung in den Herstellungsmethoden mit der Verwendung bester Materialien und bieten Ihnen dadurch Gebärbecken von unverwechselbarer Qualität. Unsere Produkte sind mit einer zwanzigjährigen Garantie versehen – auch darin sind sie außergewöhnlich

Wir haben uns bei der Weiterentwicklung der Produkte an ergonomischen Prinzipien orientiert und die konkreten Erfahrungen einbezogen, die Mütter und Hebammen mit den Gebärbecken gemacht haben
Sie bieten Müttern ausreichend Raum, um verschiedene Positionen auszuprobieren und diejenige zu finden, die für den Gebärvorgang am vorteilhaftesten ist
Hebammen können sich entspannt um die Mütter kümmern und sich darauf verlassen, dass bei der Gestaltung des Beckens jede erdenkliche geburtshilfliche Maßnahme berücksichtigt worden ist

Jedes Becken wird als nahtloses, solides Stück aus einem Guss handgefertigt und besteht aus Ficore® Verbundstruktur, einem patentierten Material von außergewöhnlicher Stabilität und Festigkeit, das sich angenehm, glatt und warm anfühlt
Mütter können über ein mehrfarbiges LED-Lichtsystem per Fernbedienung das Ambiente im Zimmer bestimmen und auf dem eingebauten Soundsystem mit Bluetooth-Empfänger ihre Lieblingsmusik abspielen
Jedes Detail des Designs, der Technik und der Fertigung ist mit dem Ziel gestaltet worden, Gebärbecken von außergewöhnlicher Qualität und höchster Wertbeständigkeit zu schaffen
Dieses kurze, einfache Video wurde auf YouTube bereits fast 12.000.000 Mal aufgerufen.
Es zeigt, wie Mütter instinktiv mit unseren Becken umgehen und sich natürlich bewegen, um die bequemsten und vorteilhaftesten Positionen zu finden.
Freiheit der Bewegung” erreicht 12.000.000 Aufrufe auf YouTube!
Obrigado pelo seu interesse em nossas piscinas de parto na água.
Nós ajudamos a pioneirar o uso de água para o trabalho de parto e nascimento ao projetar as piscinas de parto na água que tornaram essa revolução no cuidado com a maternidade possível.
Ao longo dos últimos 37 anos, fornecemos milhares de piscinas de parto na água para hospitais, centros de parto e unidades de obstetrícia ao redor do mundo, e ajudamos milhões de mulheres a terem partos melhores.
A combinação de design ergonômico baseado em evidências, centrado no usuário, materiais altamente especializados e fabricação sob medida resulta em piscinas de parto na água que estão em uma classe própria.
Alcançamos sucesso continuamente inovando, mantendo as coisas simples e focando em nossos princípios fundamentais de segurança, valor e desempenho.
Nosso entendimento único e dedicação de longo prazo em atender às necessidades das mães e parteiras nos torna singularmente qualificados para ser de serviço.
Somos recipientes de um Prêmio de Melhoria no Cuidado com a Saúde e um Prêmio Europeu de Design e amplamente reconhecidos como a escolha preferida de hospitais em todo o mundo.
Nossas piscinas de parto na água são feitas à mão por artesãos altamente qualificados na Inglaterra e construídas com um padrão tão alto que fornecem décadas de serviço e são garantidas por toda a vida.
Para uma cópia do nosso catálogo, planos e mais informações detalhadas, veja os artigos nesta página: https://activebirthpools.com/blog/?category_name=portugues
Por favor, entre em contato conosco para saber mais e obter um orçamento.
Aguardamos ansiosamente o seu contato.
#partonaágua #piscinadepartonaágua #piscinadenascimento #banhodeparto
Desde sua fundação em 1987, a Active Birth Pools tem estado na vanguarda do design e fornecimento de piscinas de parto na água.
Nosso compromisso com piscinas de parto ergonômicas, seguras e de alta qualidade nos tornou uma escolha preferida para instalações de saúde em todo o mundo.
Materiais Sustentáveis e Produção
A Active Birth Pools enfatiza a sustentabilidade através do uso do compósito Ficore®, um material conhecido por sua longevidade, durabilidade e resistência a produtos químicos e bactérias.
Com uma expectativa de vida superior a 25 anos, ele supera a durabilidade dos materiais tipicamente usados na fabricação de piscinas de parto.
As piscinas são feitas à mão na Inglaterra por artesãos qualificados, garantindo uma pegada de carbono reduzida e apoio ao emprego local.

Parteiras no Royal Berkshire Hospital comemoram o 25º aniversário de sua instalação de parto na água.
Este modelo inicial fornecido em 1992 ainda está em pleno funcionamento.
Sustentabilidade do Produto
O design das Active Birth Pools foca em durabilidade e longevidade, visando reduzir o desperdício e o uso de recursos ao longo do tempo.
O alto fator de isolamento do Ficore® e a construção de parede dupla garantem uma melhor retenção de calor, reduzindo o consumo de energia para manter a temperatura da água.
Design Ergonômico e Centrado no Usuário
Em colaboração com parteiras, obstetras e especialistas em ergonomia, desenvolvemos designs que atendem ao conforto das mães e profissionais de saúde.
Esta abordagem está alinhada com os princípios de design centrado no humano e contribui para o bem-estar e segurança dos usuários, aprimorando a experiência geral do parto.

Parteiras no `Bronte Birth Centre celebram a abertura de sua instalação de parto na água em sua nova Piscina Venus
Benefícios Econômicos
As Active Birth Pools são economicamente vantajosas para instalações de saúde devido à sua durabilidade e baixa necessidade de manutenção.
Elas também contribuem para reduzir estadias hospitalares e intervenções, levando a economias para os sistemas de saúde.
Responsabilidade Social
Segurança e satisfação do cliente são primordiais no design dessas piscinas, atendendo às necessidades de mães, bebês e trabalhadores da saúde.
O feedback positivo de uma clientela global sublinha nosso compromisso com a qualidade e segurança.

Conclusão
As Active Birth Pools demonstram um profundo compromisso com a sustentabilidade com seus materiais duráveis, designs ergonômicos e práticas de produção eficientes.
Nossa abordagem beneficia o meio ambiente e promove a sustentabilidade econômica e social na área da saúde.
As piscinas têm garantia vitalícia, superando outras no mercado em termos de segurança, higiene e satisfação do usuário.
Elas são construídas para durar décadas, economizando até £20.000 ao longo da vida útil da piscina devido à sua longevidade estendida e custos reduzidos de manutenção e energia.
As Active Birth Pools não oferecem apenas economia financeira, mas também reduzem o impacto ambiental através de menos desperdício e uso eficiente de recursos.
Elas se tornaram uma escolha favorecida em unidades de maternidade, influenciando frequentemente a escolha da instalação pelas mães.
Parteiras elogiam as piscinas por seu conforto e segurança, e os hospitais relatam que mães que usam essas piscinas experimentam partos mais fáceis e diretos, levando a estadias hospitalares reduzidas e mais economias econômicas e ambientais.
Em resumo, as Active Birth Pools se destacam como a opção mais sustentável no mercado, contribuindo significativamente para a normalização e empoderamento do processo de parto.
O vídeo “Liberdade de Movimento” alcança 12.000.000 de visualizações no YouTube!
O pináculo do design e desenvolvimento das piscinas de nascimento
Active Birth Pools ofrece la Piscina de Parto en Agua Active II/360 con Columna de Agua Personalizada, una solución sofisticada diseñada para instalaciones de atención médica que buscan proporcionar una atención materna ejemplar.
Esta combinación avanzada integra una piscina de parto en agua de última generación con una columna de agua funcional y elegante, epitomizando lo último en innovación de diseño y tecnología de materiales para el sector de atención materna.
Desarrollo Avanzado para las Necesidades de la Atención Médica Moderna
La Piscina de Parto en Agua Active II/360, un producto de Active Birth Pools, está diseñada para satisfacer las demandas en constante evolución de la atención materna contemporánea.
Complementada con la Columna de Agua Personalizada, este sistema es el resultado de una extensa investigación y colaboración con profesionales de la salud.
El enfoque ha sido crear una solución que ofrezca funcionalidad superior, seguridad y comodidad, al tiempo que aborda las necesidades prácticas tanto de los proveedores de atención médica como de las madres.

Diseño Ergonómico para una Experiencia Mejorada
La Piscina de Parto en Agua Active II/360 está diseñada con énfasis en la excelencia ergonómica y la eficiencia espacial.
La forma de cerradura de la piscina no solo es visualmente atractiva, sino que también brinda beneficios funcionales, admitiendo una variedad de posiciones y movimientos de parto.
La piscina incluye asas empotradas y un borde en forma de bull-nose para brindar un mayor soporte y seguridad.
La Columna de Agua Personalizada se integra perfectamente, ofreciendo una solución elegante para la plomería y los accesorios necesarios, mejorando así la utilidad y la estética de la piscina.

Calidad Superior del Material
Construida a partir de Ficore®, un material compuesto patentado exclusivo de Active Birth Pools, la Active II/360 ofrece una durabilidad, higiene y seguridad excepcionales.
La superficie altamente pulida y ultra suave del material es menos resbaladiza, lo que es crucial para garantizar la seguridad.
La Columna de Agua, fabricada con el mismo material de alta calidad, complementa el diseño de la piscina y mantiene los altos estándares de higiene requeridos en entornos de atención médica.

Características Centradas en el Usuario
La Piscina de Parto en Agua Active II/360 con la Columna de Agua incluye un asiento de apoyo para el trabajo de parto, facilitando una posición óptima y comodidad para la madre, y un asiento de seguridad a nivel del borde para la monitorización y evacuaciones de emergencia.
El diseño de la piscina permite el movimiento libre, lo cual es esencial para el uso efectivo de la inmersión en agua durante el trabajo de parto.
La Columna de Agua agrega funcionalidad como una estructura de soporte estable y una plataforma de utilidad práctica.

Integración de Mejoras Tecnológicas
La piscina está equipada con iluminación LED multicolor y sistemas de sonido Bluetooth, lo que permite la creación de un entorno personalizado y relajante.
Estas características son fundamentales para establecer una atmósfera de apoyo que favorezca el parto natural.

Sostenibilidad y Beneficios Económicos
El diseño duradero de la Piscina de Parto en Agua Active II/360 con Columna de Agua Personalizada la convierte en una opción sostenible y económicamente sólida para las instalaciones de atención médica.
Su rendimiento a largo plazo y la reducción de la necesidad de reemplazos frecuentes hacen de ella una inversión eficiente, alineada con los objetivos económicos y ambientales de las instituciones de atención médica modernas.

Adopción y Reconocimiento Global
La Piscina de Parto en Agua Active II/360 con Columna de Agua Personalizada ha sido reconocida a nivel mundial por su enfoque innovador en la atención materna.
Su adopción por parte de instalaciones de atención médica en todo el mundo es un testimonio de su eficacia, confiabilidad y compromiso con el avance de las prácticas de parto en agua.
En conclusión, la Piscina de Parto en Agua Active II/360 con Columna de Agua Personalizada de Active Birth Pools representa una fusión armoniosa de diseño avanzado, tecnología de material superior y una cuidadosa integración de características centradas en el usuario.
Es una elección estratégica e innovadora para las instalaciones de atención médica que buscan ofrecer una experiencia de atención materna superior, brindando comodidad, seguridad y eficiencia en un paquete integral y elegante.
Active II/360 Water Birth Pool – Hoja de Datos


Para ver cómo se vería la Piscina de Parto en Agua Active II/360 en su sala de partos, haga clic en el banner a continuación con su teléfono o tableta.
Active Birth Pools, fundada em 1987, possui uma rica história de pioneirismo e revolução no uso da água para o trabalho de parto e nascimento.
Com foco em segurança, valor e desempenho, a Active Birth Pools tornou-se a escolha principal de parteiras e hospitais em todo o mundo.
Este artigo explora por que a Active Birth Pools se destaca no mercado, tirando insights do catálogo de alta resolução da empresa, folheto e outros recursos valiosos.
Design e Ergonomia Superiores
A Active Birth Pools tem continuamente evoluído seus designs em colaboração com parteiras, mães, obstetras e especialistas em saúde e segurança.
Esta abordagem colaborativa levou ao primeiro pool de nascimento hospitalar especialmente projetado do mundo.
Os pools apresentam designs ergonômicos que priorizam o conforto tanto das mães quanto das parteiras.
Por exemplo, os pools oferecem uma borda larga para que as parteiras possam descansar seus braços e pernas confortavelmente, semelhante a sentar-se em uma mesa.
As mães se beneficiam de várias posições suportadas, incluindo sentar, ajoelhar e agachar, graças às bordas moldadas do pool.

Qualidade do Material e Durabilidade
Os pools são fabricados a partir do Ficore®, um material proprietário com qualidades únicas, tornando-os mais duráveis, práticos e seguros em comparação com outros materiais.
Os pools Ficore® apresentam retenção de calor superior, reduzindo a perda de calor para apenas 0,7 graus por hora, o que é altamente benéfico durante o trabalho de parto prolongado.
Além disso, o material é resistente a bactérias, agentes de limpeza e desinfetantes fortes, garantindo altos padrões de higiene e segurança.
Segurança e Higiene
O design da Active Birth Pools minimiza o risco de lesões com recursos como resistência ao escorregamento e superfícies menos escorregadias.
A construção de uma única peça de Ficore® aumenta a segurança e higiene da água, prevenindo o crescimento de bactérias no ambiente.
Além disso, a construção sem emendas e superfícies lisas eliminam “armadilhas para sujeira” e facilitam a limpeza e manutenção mais eficazes.

Conforto e Suporte
Os designs da Active Birth Pools são centrados no conforto e apoio às mães.
A flutuabilidade da água nos pools suporta o peso do corpo da mãe, permitindo relaxamento e facilidade durante o trabalho de parto.
Essa flutuabilidade também facilita para as mães adotar e mudar entre posições eretas ou agachadas, que são conhecidas por serem benéficas durante o trabalho de parto.
Feedback Positivo e Endossos
A empresa recebeu inúmeros depoimentos positivos de parteiras, profissionais de saúde e mães.
Esses depoimentos destacam o conforto, facilidade de uso, segurança e praticidade dos pools.
Tais endossos são um testemunho do compromisso da empresa com a qualidade e a satisfação do usuário.
Recursos Inovadores
A Active Birth Pools integrou recursos modernos, como iluminação LED multicolorida e sistemas de som Bluetooth em seus pools.
Esses recursos criam uma atmosfera propícia para o trabalho de parto fisiológico e parto natural, aprimorando a experiência geral do parto.
Longevidade e Sustentabilidade
Uma grande vantagem da Active Birth Pools é sua durabilidade e sustentabilidade.
Pools feitos de Ficore® têm uma expectativa de vida superior a 25 anos, tornando-os uma opção mais sustentável em comparação com outros pools de parto na água com vida útil mais curta.

Conclusão
A Active Birth Pools se destaca como uma escolha de primeira linha para parteiras e hospitais devido à sua dedicação à qualidade, segurança e inovação.
A abordagem da empresa ao design ergonômico, aliada ao uso de materiais superiores e atenção ao feedback do usuário, a posiciona como líder no mercado de pools de parto na água.
Com seus pools, hospitais e centros de parto podem oferecer um ambiente de parto mais seguro, confortável e sustentável, levando a melhores resultados tanto para as mães quanto para as parteiras.
O pináculo do design e desenvolvimento das piscinas de nascimento
O vídeo “Liberdade de Movimento” alcança 12.000.000 de visualizações no YouTube!
Piscinas de Parto Activo, fundada en 1987, ha desempeñado un papel pionero en el uso del agua durante el trabajo de parto y el parto.
Sus valores y enfoque pueden comprenderse de manera integral al examinar varios aspectos de sus operaciones y productos.

Innovación y Espíritu Pionero:
Piscinas de Parto Activo ayudó a pionerar el uso del agua en el trabajo de parto y el parto, trabajando en estrecha colaboración con parteras, madres, obstetras y expertos en control de infecciones y manejo manual.
Este enfoque colaborativo llevó al desarrollo de la primera piscina de parto de grado hospitalario especialmente diseñada en el mundo, demostrando su compromiso con la innovación y la mejora en la atención materna.
Seguridad, Valor y Rendimiento:
La empresa enfatiza estos principios fundamentales en sus productos.
Se centran en la producción de piscinas de parto que sean seguras, ofrezcan un gran valor y funcionen de manera excepcional.
Este enfoque se refleja en el uso de materiales especializados como el Ficore®, un material patentado conocido por su durabilidad, practicidad y características de seguridad.
Por ejemplo, las piscinas Ficore® retienen el calor de manera eficiente y son resistentes a las bacterias y a los desinfectantes fuertes, garantizando altos estándares de higiene.

Diseño Ergonómico:
Piscinas de Parto Activo emplea principios de diseño ergonómico basados en evidencia y centrados en el usuario.
Sus piscinas están diseñadas para satisfacer las necesidades de comodidad tanto de las madres como de las parteras, con diseños que admiten diversas posiciones como sentarse, arrodillarse y ponerse en cuclillas.
Los amplios bordes de las piscinas permiten que las parteras descansen cómodamente, similar a sentarse en un escritorio, lo que demuestra su consideración tanto por la comodidad de los usuarios como por la practicidad.
Opiniones de los Clientes y Recomendaciones:
La empresa valora los comentarios de los clientes y ha recibido numerosos testimonios positivos de profesionales de la salud y madres.
Estos testimonios a menudo destacan la comodidad, facilidad de uso, seguridad y practicidad de las piscinas, lo que refleja la dedicación de la empresa a la calidad y la satisfacción del usuario.

Calidad de Construcción y Garantía:
Las piscinas de Parto Activo se fabrican a mano bajo pedido en Inglaterra por artesanos altamente capacitados que se enorgullecen de su trabajo y están dedicados a la excelencia.
Piscinas de Parto Activo ofrece una garantía de por vida en sus piscinas de parto en agua, lo que refleja su compromiso con la calidad y la durabilidad.
Esta garantía de por vida es un testimonio de la confianza que la empresa deposita en su diseño, materiales y procesos de fabricación.
Sostenibilidad y Longevidad:
Piscinas de Parto Activo otorga importancia a la sostenibilidad.
Sus piscinas tienen una esperanza de vida que supera los 25 años, lo que las convierte en una opción sostenible en comparación con otras piscinas de parto que tienen vidas útiles más cortas.
Esta longevidad no solo proporciona una buena relación calidad-precio, sino que también se alinea con los principios de sostenibilidad ambiental.

Alcance Global y Experiencia:
Con una historia que abarca varias décadas, Piscinas de Parto Activo ha suministrado miles de piscinas de parto en agua en todo el mundo.
Su amplia experiencia y conocimiento en el campo los han convertido en la opción líder para hospitales y parteras a nivel mundial.
Este alcance global subraya su compromiso con la mejora de la atención materna a nivel global.
En resumen, los valores de Piscinas de Parto Activo se centran en la innovación, la seguridad, el diseño ergonómico, la satisfacción del cliente, la sostenibilidad y una perspectiva global para mejorar la atención materna.
Estos valores han guiado sus operaciones y el desarrollo de productos, posicionándolos como líderes en el mercado de piscinas de parto en agua.
No cenário em constante evolução do cuidado materno, os hospitais estão continuamente buscando maneiras inovadoras de aprimorar a experiência de parto para as mães grávidas.
Uma inovação que está ganhando impulso é a integração de piscinas de parto aquáticas nas instalações hospitalares.
Longe de ser apenas uma tendência passageira, as piscinas de parto aquáticas oferecem uma miríade de benefícios que não apenas priorizam o bem-estar tanto da mãe quanto do bebê, mas também contribuem para uma experiência de parto mais holística e capacitadora.
Neste artigo, exploramos as razões convincentes pelas quais os hospitais deveriam considerar abraçar a maré e incorporar piscinas de parto aquáticas em seus serviços de cuidado materno.

Alívio Natural da Dor:
A água é reconhecida há muito tempo como um poderoso analgésico natural.
Imersão em água morna pode aliviar a intensidade das contrações e proporcionar uma sensação de leveza, reduzindo o impacto da gravidade no corpo.
Hospitais que oferecem piscinas de parto aquáticas proporcionam às mães uma opção alternativa de gerenciamento da dor que complementa métodos tradicionais, oferecendo uma abordagem mais personalizada ao conforto durante o trabalho de parto.
Numerosos estudos demonstraram a eficácia da imersão em água para aliviar a dor do trabalho de parto.
Uma revisão publicada no “Journal of Perinatal Education” (Harper et al., 2016) concluiu que a imersão em água morna durante o trabalho de parto reduz significativamente a percepção da dor, proporcionando às mães expectantes uma opção de alívio da dor não farmacológica e baseada em evidências.
Pesquisas publicadas no “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) sugerem que a imersão em água durante o trabalho de parto reduz os hormônios do estresse, promovendo um estado mais relaxado tanto para a mãe quanto para o bebê.
Níveis mais baixos de hormônios do estresse têm sido associados a um melhor bem-estar materno e resultados de parto favoráveis, apoiando o argumento das piscinas de parto aquáticas como uma abordagem holística ao cuidado materno.

Redução do Estresse e Ansiedade:
O processo de parto pode ser uma fonte de ansiedade para muitas mães grávidas.
As piscinas de parto aquáticas criam um ambiente tranquilo e relaxante, promovendo a relaxamento e reduzindo os níveis de estresse.
A flutuabilidade da água promove uma sensação de leveza, permitindo que as mães se movam mais livremente e adotem posições confortáveis, contribuindo para uma experiência de parto mais positiva e capacitadora.
Pesquisas publicadas no “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) sugerem que a imersão em água durante o trabalho de parto reduz os hormônios do estresse, promovendo um estado mais relaxado tanto para a mãe quanto para o bebê.
Níveis mais baixos de hormônios do estresse têm sido associados a um melhor bem-estar materno e resultados de parto favoráveis, apoiando o argumento das piscinas de parto aquáticas como uma abordagem holística ao cuidado materno.

Facilitação do Movimento e Posicionamento:
As piscinas de parto aquáticas proporcionam um ambiente propício para o movimento e posicionamento durante o trabalho de parto.
A flutuabilidade permite uma mobilidade aumentada, possibilitando que as mães mudem de posição facilmente e encontrem a postura mais confortável para o parto.
Essa flexibilidade pode aprimorar o progresso do trabalho de parto e facilitar um processo de parto mais suave.
Um estudo publicado no “American Journal of Obstetrics & Gynecology” (Zanetti-Daellenbach et al., 2007) descobriu que a imersão em água melhora a mobilidade materna durante o trabalho de parto.
A flutuabilidade da água permite um movimento e posicionamento mais fáceis, potencialmente encurtando a duração do trabalho de parto e reduzindo a necessidade de intervenções.
Esta evidência destaca a importância das piscinas de parto aquáticas ao proporcionar um ambiente propício para posições de parto ideais.

Melhor Circulação Sanguínea:
A água morna em uma piscina de parto promove uma melhor circulação sanguínea, o que pode ser particularmente benéfico durante o trabalho de parto.
A circulação aprimorada ajuda a reduzir o inchaço e promove o fluxo de oxigênio, contribuindo para o bem-estar tanto da mãe quanto do bebê.
Hospitais que incorporam piscinas de parto aquáticas priorizam os aspectos fisiológicos do parto, promovendo um ambiente de parto mais saudável.
O impacto positivo da imersão em água morna na circulação sanguínea é bem documentado.
Um ensaio clínico randomizado publicado no “Journal of Midwifery & Women’s Health” (Burns et al., 2012) revelou que a imersão em água morna aumenta o fluxo sanguíneo periférico e a oxigenação, proporcionando benefícios fisiológicos que contribuem para o bem-estar global tanto da mãe quanto do bebê.

Fortalecimento do Vínculo:
O ambiente íntimo e privado de uma piscina de parto aquática incentiva o envolvimento do parceiro e promove uma conexão mais profunda entre os pais e o recém-nascido.
A experiência compartilhada de trabalho de parto e parto em uma piscina de parto pode fortalecer o vínculo emocional entre os parceiros, promovendo um senso de unidade e responsabilidade compartilhada ao receber o mais novo membro da família.
Uma análise meta-abrangente publicada em “Birth: Issues in Perinatal Care” (Nikodem et al., 2016) examinou os resultados psicológicos da imersão em água durante o trabalho de parto.
A análise encontrou uma correlação positiva entre as experiências de parto em água e o aumento da satisfação materna e do vínculo com o recém-nascido.

Conclusão:
Hospitais que priorizam a inclusão de piscinas de parto aquáticas estão alinhados com evidências que apoiam os benefícios emocionais desta abordagem ao parto.
A inclusão de piscinas de parto aquáticas nos serviços de cuidado materno do hospital representa um passo progressivo em direção a uma abordagem mais abrangente e centrada no paciente para o parto.
Além dos benefícios físicos, como alívio natural da dor e circulação aprimorada, as piscinas de parto aquáticas contribuem para uma experiência emocionalmente enriquecedora para ambos os pais.
À medida que os hospitais se esforçam para priorizar o bem-estar e as preferências das mães grávidas, a integração de piscinas de parto aquáticas surge como uma escolha convincente, ecoando a antiga conexão entre a humanidade e o abraço reconfortante da água durante o milagre do parto.
Incorporar piscinas de parto aquáticas nos serviços de cuidado materno do hospital não é apenas um passo progressivo; é um salto respaldado cientificamente em direção a experiências de parto centradas em evidências.
A multiplicidade de estudos que apoiam os benefícios da imersão em água durante o trabalho de parto reforça a ideia de que os hospitais devem considerar as piscinas de parto aquáticas não como um luxo, mas como um elemento crucial para promover um ambiente de parto seguro, confortável e baseado em evidências.
A maré de evidências apoia esmagadoramente a integração de piscinas de parto aquáticas como uma força transformadora na moderna assistência materna.
O pináculo do design e desenvolvimento das piscinas de nascimento
O vídeo “Liberdade de Movimento” alcança 12.000.000 de visualizações no YouTube!
Abraçando a Maré: O Compelente Argumento para Piscinas de Parto Aquáticas em Hospitais
En el siempre cambiante panorama de la atención materna, los hospitales buscan continuamente formas innovadoras de mejorar la experiencia de parto para las futuras madres.
Una innovación que está ganando impulso es la integración de piscinas de parto en el agua dentro de las instalaciones hospitalarias.
Lejos de ser una simple tendencia, las piscinas de parto en el agua ofrecen una miríada de beneficios que no solo priorizan el bienestar tanto de la madre como del niño, sino que también contribuyen a una experiencia de parto más holística y empoderadora.
En este artículo, nos adentramos en las razones convincentes por las cuales los hospitales deberían considerar abrazar la marea e incorporar piscinas de parto en el agua en sus servicios de atención materna.

Alivio Natural del Dolor:
El agua ha sido reconocida durante mucho tiempo como un potente analgésico natural.
Sumergirse en agua tibia puede aliviar la intensidad de las contracciones y proporcionar una sensación de ingravidez, reduciendo el impacto de la gravedad en el cuerpo.
Los hospitales que ofrecen piscinas de parto en el agua brindan a las madres una opción alternativa de manejo del dolor que complementa los métodos tradicionales, ofreciendo un enfoque más personalizado para el confort durante el trabajo de parto.
Numerosos estudios han demostrado la eficacia de la inmersión en agua para aliviar el dolor del parto.
Una revisión publicada en el “Journal of Perinatal Education” (Harper et al., 2016) concluyó que la inmersión en agua tibia durante el trabajo de parto reduce significativamente la percepción del dolor, proporcionando a las futuras madres una opción de alivio del dolor no farmacológica y basada en evidencia.
La investigación publicada en el “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) sugiere que la inmersión en agua durante el trabajo de parto reduce las hormonas del estrés, promoviendo un estado más relajado tanto para la madre como para el bebé.
Niveles más bajos de hormonas del estrés se han asociado con una mejora en el bienestar materno y resultados de parto favorables, respaldando el argumento a favor de las piscinas de parto en agua como enfoque holístico para la atención materna.

Reducción del Estrés y la Ansiedad:
El proceso de parto puede ser una fuente de ansiedad para muchas futuras madres.
Las piscinas de parto en agua crean un entorno tranquilo y relajante, fomentando la relajación y reduciendo los niveles de estrés.
La flotabilidad del agua promueve una sensación de ingravidez, permitiendo que las madres se muevan con más libertad y adopten posiciones cómodas, contribuyendo a una experiencia de parto más positiva y empoderadora.
La investigación publicada en el “Journal of Obstetric, Gynecologic & Neonatal Nursing” (Thoeni et al., 2019) sugiere que la inmersión en agua durante el trabajo de parto reduce las hormonas del estrés, promoviendo un estado más relajado tanto para la madre como para el bebé.
Niveles más bajos de hormonas del estrés se han asociado con una mejora en el bienestar materno y resultados de parto favorables, respaldando el argumento a favor de las piscinas de parto en agua como enfoque holístico para la atención materna.

Facilitación del Movimiento y la Posición:
Las piscinas de parto en agua proporcionan un entorno propicio para el movimiento y la posición durante el trabajo de parto.
La flotabilidad permite una mayor movilidad, permitiendo que las madres cambien de posición fácilmente y encuentren la postura más cómoda para el parto.
Esta flexibilidad puede mejorar el progreso del trabajo de parto y facilitar un proceso de parto más suave.
Un estudio publicado en el “American Journal of Obstetrics & Gynecology” (Zanetti-Daellenbach et al., 2007) encontró que la inmersión en agua mejora la movilidad materna durante el trabajo de parto.
La flotabilidad del agua permite un movimiento y posicionamiento más fáciles, acortando potencialmente la duración del trabajo de parto y reduciendo la necesidad de intervenciones.
Esta evidencia subraya la importancia de las piscinas de parto en agua al proporcionar un entorno propicio para las posiciones óptimas de parto.

Mejora de la Circulación Sanguínea:
El agua tibia en una piscina de parto promueve una mejora en la circulación sanguínea, lo cual puede ser particularmente beneficioso durante el trabajo de parto.
Una circulación mejorada ayuda a reducir la hinchazón y promover el flujo de oxígeno, contribuyendo al bienestar tanto de la madre como del bebé.
Los hospitales que incorporan piscinas de parto en agua priorizan los aspectos fisiológicos del parto, promoviendo un entorno de parto más saludable.
El impacto positivo de la inmersión en agua tibia en la circulación sanguínea ha sido bien documentado.
Un ensayo controlado aleatorio publicado en el “Journal of Midwifery & Women’s Health” (Burns et al., 2012) reveló que la inmersión en agua tibia aumenta el flujo sanguíneo periférico y la oxigenación, proporcionando beneficios fisiológicos que contribuyen al bienestar general tanto de la madre como del bebé.

Mejora del Vínculo:
El entorno íntimo y privado de una piscina de parto en agua fomenta la participación de la pareja y promueve una conexión más profunda entre los padres y el recién nacido.
La experiencia compartida del trabajo de parto y el parto en una piscina de parto en agua puede fortalecer el vínculo emocional entre los compañeros, promoviendo una sensación de unidad y responsabilidad compartida al dar la bienvenida al miembro más nuevo de la familia.
Un exhaustivo metaanálisis publicado en “Birth: Issues in Perinatal Care” (Nikodem et al., 2016) examinó los resultados psicológicos de la inmersión en agua durante el trabajo de parto.
El análisis encontró una correlación positiva entre las experiencias de parto en agua y un aumento en la satisfacción materna y en el vínc

La inclusión de piscinas de parto en agua en los servicios de atención materna hospitalaria representa un paso progresivo hacia la implementación de un enfoque más integral y centrado en el paciente para el parto.
Más allá de los beneficios físicos, como el alivio natural del dolor y la mejora de la circulación, las piscinas de parto en agua contribuyen a una experiencia más enriquecedora emocionalmente para ambos padres.
A medida que los hospitales se esfuerzan por priorizar el bienestar y las preferencias de las futuras madres, la integración de piscinas de parto en agua se presenta como una elección convincente, resonando con la conexión ancestral entre la humanidad y el abrazo tranquilizador del agua durante el milagro del parto.
Incorporar piscinas de parto en agua en los servicios de atención materna hospitalaria no es simplemente un paso progresivo; es un salto respaldado científicamente hacia la provisión de experiencias de parto basadas en evidencia y centradas en el paciente.
La multitud de estudios que respaldan los beneficios de la inmersión en agua durante el trabajo de parto refuerza la idea de que los hospitales deberían considerar las piscinas de parto en agua no como un lujo, sino como un elemento crucial para fomentar un entorno de parto seguro, cómodo y basado en evidencia.
La avalancha de evidencia respalda de manera abrumadora la integración de piscinas de parto en agua como una fuerza transformadora en la atención materna moderna.
La cúspide del diseño y el desarrollo de las piscinas de nacimiento en el agua.
Nada ayuda a las madres a sobrellevar el dolor en el parto de manera más efectiva
El video “Libertad de Movimiento” alcanza 12,000,00 vistas en YouTube!
Negli anni ’80, abbiamo intrapreso un viaggio insieme a ostetrici, madri, ginecologi, specialisti del controllo delle infezioni ed esperti in movimentazione manuale.
Insieme, abbiamo creato la prima piscina per il parto in acqua di grado ospedaliero al mondo, prestando la massima attenzione a ogni dettaglio.
Da allora, abbiamo continuato a perfezionare i nostri progetti, migliorare i nostri materiali e elevare le nostre capacità di produzione ed ingegneria.
Quest’evoluzione ha dato vita a piscine per il parto in acqua che non solo prioritizzano la sicurezza, ma si allineano perfettamente con i desideri sia delle madri che delle ostetriche.

I giudici dei Building Better Healthcare Awards lo hanno descritto in modo succinto, affermando che l’armoniosa fusione di progettazione basata su prove, centrata sull’utente, ergonomicità, materiali specializzati e produzione su misura ha portato a piscine per il parto in acqua che si distinguono in una categoria a parte.
La nostra dedizione incrollabile consiste nell’offrire piscine per il parto intelligentemente progettate che offrono una sicurezza ineguagliabile, un valore straordinario e prestazioni eccezionali, il tutto restando incredibilmente pratiche, convenienti e sostenibili dal punto di vista ambientale.
Al centro di tutto ciò c’è una vera passione per il design e la qualità, alimentata da un impegno incondizionato per migliorare l’esperienza del travaglio e del parto sia per le ostetriche che per le madri e i neonati.

Siamo orgogliosi di aver fornito innumerevoli piscine per il parto in acqua agli ospedali di tutto il mondo.
Le nostre collaborazioni con gli utenti finali, gli specialisti e i produttori ci hanno spinto a sviluppare e migliorare continuamente le nostre capacità.
Ogni Active Birth Pool viene realizzata artigianalmente su misura in Inghilterra da abili artigiani che sono immensamente orgogliosi del loro lavoro e che si attengono agli standard più elevati di eccellenza.

Il nostro processo di progettazione tiene conto della delicata interazione tra madri, ostetriche e la piscina per il parto.
Abbiamo abbracciato principi di progettazione basati su prove, centrati sull’utente ed ergonomici per creare piscine per il parto in acqua che sono non solo estremamente confortevoli, ma anche incredibilmente pratiche e user-friendly.
Le forme intricate e accattivanti delle nostre piscine sono progettate per catturare sia i sensi che le emozioni.
Ogni curva, ogni contorno ha uno scopo, dove la forma si fonde elegantemente con l’utilità estetica.

Attraverso il processo di fabbricazione senza soluzione di continuità in Ficore®, abbiamo rivoluzionato il concetto di piscina per il parto.
Questa innovazione ha dato vita a piscine che combinano senza soluzione di continuità eleganza, praticità e facilità d’uso.
Le eccezionali qualità di Ficore® ci consentono di produrre piscine per il parto in acqua che eccellono in termini di prestazioni, valore e sicurezza oltre misura.
La nostra profonda comprensione del processo di nascita e il nostro impegno verso le esigenze delle ostetriche ci hanno spinto a progettare piscine per il parto che proteggono attivamente le ostetriche e le madri dai potenziali rischi associati al parto in acqua..

Siamo pienamente consapevoli del potenziale delle piscine per il parto di ospitare batteri dannosi.
In risposta, abbiamo introdotto una serie di funzioni innovative che non solo mitigano il rischio, ma amplificano anche la sicurezza al massimo grado.
La vostra tranquillità e sicurezza sono al centro di tutto ciò che facciamo.
Il video “Libertà di Movimento” raggiunge 12.000.000 di visualizzazioni su YouTube!
L’apice del design e dello sviluppo delle piscine per il parto
Las piscinas de parto en agua desempeñan un papel vital en ayudar a las madres a experimentar un trabajo de parto fisiológico y un parto natural.
Nada ayuda a las madres a sobrellevar el dolor de manera más efectiva. Si las madres no van a depender de la analgesia para el alivio del dolor, necesitan otras opciones.

Las madres que ingresan a una piscina de agua tibia durante el trabajo de parto establecido encuentran que son mejores para sobrellevar el dolor.
La inmersión en agua tibia ha sido inequívocamente demostrada como de gran beneficio tanto fisiológica como psicológicamente.
Las mujeres tienen un mayor sentido de realización y logro, y los bebés experimentan un parto no traumático.
Además de los beneficios obvios para las madres y los bebés, las parteras experimentan una mayor satisfacción laboral y los hospitales ahorran dinero y optimizan recursos.
Casi un tercio de las mujeres se beneficiaron del uso de una piscina de parto en agua en el Reino Unido en 2014 (Encuesta Nacional de Maternidad 2014).

Con hasta un 60% de las madres dispuestas a un parto natural, ahora es el momento de considerar la disponibilidad más amplia de esta opción segura, efectiva y de bajo costo.
En tierra, las madres luchan contra la fuerza de gravedad, lo que limita el movimiento a medida que avanza el trabajo de parto y se cansan.
Muchas mujeres no tienen la capacidad física para mantener posturas erguidas durante largos períodos de tiempo (Gupta JK, Hofmeyr GJ, Smyth R 2007).
Las madres que tienen sobrepeso u obesidad a menudo no pueden hacer frente a las demandas físicas.
La transición de la tierra al agua ayuda a revivir y energizar a las madres, dándoles una nueva oportunidad en la vida y un sentido de propósito.
La flotación del agua apoya a la madre, reduciendo su peso relativo aproximadamente en un 33% (Principio de Arquímedes).
Esto le permite moverse de formas que no son posibles en tierra.
Para explorar y beneficiarse de las posturas naturales para el trabajo de parto y el parto. El efecto calmante y relajante del agua tibia promueve el flujo de oxitocina.

Esta poderosa hormona desempeña un papel fundamental en el parto.Hace que el útero se contraiga y desencadena el ‘reflejo de eyección fetal’.
La inmersión en agua tiene un efecto fisiológico beneficioso en la secreción de hormonas, incluyendo aumentos de oxitocina que pueden avanzar la dilatación y estimular las contracciones (Odent 2014).
La cúspide del diseño y el desarrollo de las piscinas de nacimiento en el agua.
El video “Libertad de Movimiento” alcanza 12,000,00 vistas en YouTube!
Dieses kurze Video mit über 12.000.000 Aufrufen zeigt, dass Mütter Raum haben, sich in den natürlichen Haltungen während der Geburt und bei der Entbindung frei zu bewegen.
Wie sie instinktiv mit unseren Geburtsbecken in Wasser interagieren und sich auf natürliche Weise bewegen, um die bequemsten und vorteilhaftesten Positionen zu finden.
Die Bewegungsfreiheit in Verbindung mit den entspannenden Wirkungen von warmem Wasser fördert die Freisetzung von Oxytocin, was die Wahrscheinlichkeit signifikant erhöht, dass Mütter eine physiologische Geburt und eine natürliche Entbindung erleben.