The introduction of birthing pools in the UK began in the late 1980’s and is one of the greatest innovations to happen in natural childbirth. More than 150 hospitals in the UK now (2001) have at least one installed pool and hundreds of portable pools are also in circulation. The use of water for labour and birth is increasing and has been under intense scrutiny in the last 10 years. The outcomes of the research have so far, been positive. The help of water to enable more women to give birth naturally is very relevant at this time, when one in 5 babies in the UK is born by caesarean section.
The invigorating and therapeutic value of water is well know to all of us – from our daily bath or shower to mineral springs, saunas and spa’s, rivers, oceans – all places we go to for healing and regeneration. These qualities are brought into the labour room when we introduce a pool of warm water. This is a wonderful way to transform the atmosphere in a hospital and to encourage normal birth physiology.
Long before there was modern plumbing, water was used as a birth aid in many cultures. It’s soothing, cleansing, and healing properties were used to help women in labour and it was also used as a birth stimulant.
- In New Guinea – Gahuka women gave birth by the river. The sound of the water help the mothers concentration and the flowing movement of the water helps the movement of the baby inside.
- African women – Squat over steaming hot rocks to soften the perineum
- Gautemalan midwives – gave women relaxing steam bath massages
- Finnish women laboured in steaming saunas
- Japanese women in remote fishing villages gave birth in the sea
- Maories and South Pacific Islanders – Hawaiians – have oral traditions of labour and birth in water. In addition to gravity, warm water is another of nature’s elements which has enormous power to help you during your labour. It is a simple yet powerful way to relax deeply and can be the key to an easier labour.
The benefits of using a birth pool
Water is a feminine element. It is buoyant and soft and carries your body’s weight. As soon as you enter the water, the warm, sensual sensations on your skin remind you that your labouring body is beautiful, powerful, and sensual. Although this is not the case for everyone, the majority of women comment that they were surprised by how wonderful and relieving it felt when they first got into the pool.
Water pools help many women to cope better with pain and enhances those passions and deep emotions which are an integral part of a healthy birth. For many women a birth pool provides an alternative route to an epidural and can be the key to a physiological birth. The water is not likely to take away the pain, but it can make a tremendous difference to your ability to relax and may well make the pain more bearable.
Studies have shown that endorphine levels may go down in a birth pool – a sign that pain levels decrease. A birth pool is something to try before considering an epidural or other form of medical pain relief. You can always change your mind if you need to.
The buoyant effect of the water completely supports your body’s weight. This gives you a feeling of physical liberation – like being in warm ocean. Resting between contractions is much easier, because being in the water is so comfortable and relaxing. This helps tremendously to conserve your strength and energy, so you are less likely to become fatigued or exhausted.
In the pool you are in your own womblike space – you are in charge. It’s more difficult to disturb or distract you. A birth pool represents a sanctuary from what some women experience as the menace of obstetric routines. In water your body is your own territory – your birth attendants need your consent to get close to you.
The water’s buoyancy also helps enormously to make you more comfortable in upright positions. You can move more easily and spontaneously help your baby to descend and rotate by yourself.
You will be surprised to find that it’s much easier, for example, to squat in water. Even women who find squatting difficult on land, can often do so comfortably in water — with the added benefit that this position makes a lot more space in the pelvis for your baby to descend.
Once in the pool, you are unlikely to notice how much time has passed. Many women say that the world beyond the rim of the pool seems to disappear.This increased sense of privacy in the pool helps you to concentrate on working through your contractions without any distractions.
The relaxing environment helps you to let go of what is happening around you and to focus your awareness inwards on the work your body is doing and surrender to the rhythm of your labour.
The oxytocin wave – how entering a birth pool effects hormone secretion.
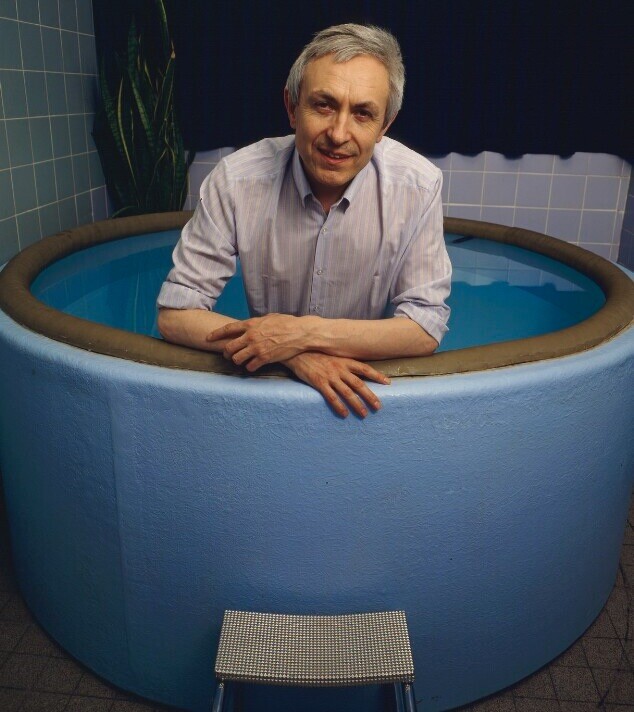
Water birth pioneer, Dr Michel Odent, in his latest updates on water birth, suggests that there is a correlation between the findings of physiologists on the effects of water immersion on hormone secretion and the observations of midwives that labours tend to slow down when the woman enters the pool too early.
He suggests that immediately after a woman enters the pool, there is a surge of oxytocin which stimulates contractions and results in rapid dilation. However this effect is short lived and after about 1.5 – 2 hours, oxytocin secretion reaches a peak and begins to slow down. The timing of when you enter the pool therefore becomes important.
Practical tips and guidelines
When to get in – If you are planning to use a birth pool it’s best to stay out of the water in the latent phase of labour. At this time, using upright positions, movement and breathing awareness, complementary therapies or TENS can help you to get into a comfortable rhythm with your labour (see Issue nos 8 and 10)
.In mid labour, when you are about 5 – 6 cms dilated – around the time when many women ask for pain relief – is the best time to think about entering a birth pool (our experience also shows that getting in too early can slow down contractions). Getting in late means that you are likely to be close to full dilation at the crest of the oxytocin wave.
In a long labour, contractions may slow down in the pool and then it is best get out and use the help of gravity on dry land for a while, resting in the pool later if you get tired.
The golden rule of water labour and birth – if progress is slow in water try land, if slow on land try water
The water temperature is important. Because your baby relies on you for temperature regulation and is one degree warmer than you are, the temperature of the water should never exceed 36C in labour and is best at 36C or 37C for the birth itself. When you feel cold, hormone secretion is inhibited and this will weaken your contractions. If you feel warm enough but not hot, you have probably got it just right for you. Measuring the temperature with a water thermometer is important, but don’t worry about it being too exact! How you feel is the best test.
The ideal water temperature range in labour is 32C-36C and for birth around 36C-37C
Water depth – You also need to make sure that in labour the water is deep enough to cover your belly and allow your shoulders to be exposed, so you can sweat and loose heat if you need to. Immediately after the birth there is often a need to remove some of the water, so you can breastfeed in the pool with the water keeping your baby’s body warm with his or her head out of the water at breast level.
Birthing rooms with a pool are warm and humid, so make sure that there is good ventilation and the room is not over heated. Plenty of drinking water for everyone is also a good idea, as a humid atmosphere is dehydrating.
Your partner can sit right beside you in the pool or even get in with you to massage, hold and comfort you. As you share the same environment, there is no increased risk of infection if your partner enters the pool! So it’s a good idea to have a swimsuit ready for your partner, just in case.
If this idea doesn’t appeal to you, it’s still very easy to share the intimacy of labour with your partner seated nearby, outside the pool. Having a low stool or a birth ball beside the pool is useful for your partner and for the midwife. Many women value having all the space in the pool to themselves, while others enjoy the comfort and support of relaxing against their partner’s body in the water.
* The Midwife’s practise
It is a transforming experience for a midwife to be around women in a birth pool. It is understandable that midwives contemplating their first water births may be nervous and feel insecure. Until very recently their education would not have included Water Birth. The health authority generally prefer two midwives to be at a water birth.
The fact that you are in water does not greatly change the midwife’s usual practice – in fact it makes it considerably easier, because the warm water helps you to cope better by yourself. She will need to make the normal observations of both your and your baby’s well being and the progress of your labour.
Vaginal exams can be kept to a minimum and can be done when necessary in the pool.
Monitoring the baby’s heartbeat at regular (probably half hourly) intervals is important to ensure that there is no foetal distress. However the midwife needs to be sensitive to avoid disturbing you too much – a waterproof sonic aid allows monitoring under water so you do not need to change your position or break your concentration. Alternatives are a stethoscope, a long stemmed pinnard or a regular sonic aid with the transducer in the finger of a long glove. A non water proof sonic aid may mean that you need to float close to the edge or sit up on the edge of the pool.
The midwife will check your body temperature and blood pressure at times and keep an eye on the temperature of the water.
When a birth pool is introduced into a hospital birthing room the environment is transformed into one which is much more homelike. The pool invites the mother to relax and there is usually no delivery bed in sight. The atmosphere of fear and danger are eradicated and everyone’s expectations about what will happen are different. There is a deliberate attempt to induce feelings of confidence and relaxation in the mother.
This makes a hospital environment more attractive if you want a physiological birth with the security of obstetric support close at hand. At a home birth the environment is even more ‘hormone enhancing’ when a birth pool is available and there is a powerful resource to help you cope with pain in the active stage of labour.
In the pool room it’s a good idea to dim the lights or draw the curtains to reduce stimulation so that there is a peaceful, calm and intimate atmosphere. When you can really relax in labour, as a birth pool helps you to do – you can let go more easily and things usually go well. It’s not a problem if you want or need to get out for the birth. You will have achieved the most important objective, which is a more comfortable labour, without the need for drugs or interventions.
How to use Water during Labour:
How long and When to Stay in the Water
The attraction to water and the timing of using the water pool is very individual and varies from one woman to another and one labour to another. If pre-labour contractions are intense and there are long runs of contractions prior to the onset of established labour, water can be extremely soothing.
After staying in water for some time the contractions may diminish, giving you an opportunity to rest and maybe even fall asleep, thus conserving your energy for the subsequent labour and birth.
When labour is well established, the timing of using the pool once again shows a wide individual variation. After entering the water dilation is often rapid during the first h our. It is preferable to keep the pool in reserve for the second half of labour when the contractions are intense and the periods of rest shorter.
This is when water is most powerful in assisting dilation and shortening labour. However, you might need the comfort of water from quite early on in labour and want to spend hours in the pool prior to the birth itself. In this instance you can go in and out of the pool and alternate between being in water and being on land.
When the pool is used early, mothers sometimes tire of the water and they may not want to use this valuable resource later on when contractions become more painful and intense. Getting in too early may slow down contractions and prolong labour.
Provided the correct water temperature is maintained and your temperature is monitored, it is safe to stay in the water as long as you like. The depth of the water is also important. The more your body is submerged the more help you will get from buoyancy.
However, women’s preferences vary. While some like the water to be as deep as possible, others are more comfortable in less water.
When you leave the pool it is advisable to have plenty of large towels available so that you can dry yourself completely. There should also be a heater in the room so that if you feel cold the temperature can be raised quickly.
Movements and Positions
There are bound to be times when you prefer to need to be outside the pool on dry land during your labour, for example, if labour is not progressing well in water or if you do not feel like being in water. In early labour, as your contractions are beginning to intensify it is essential to make the most of the help of gravity.
You can do this by using positions such as standing, sitting or squatting during your contractions and resting between them. Follow you instincts when moving during labour and you will find that these positions occur spontaneously.
Most women use a variety of positions. Some prefer one or two while other women are more restless and change position frequently. During contractions movements such as circling your hips or rocking your pelvis can help to dissipate the pain.
There are many ways to make yourself comfortable in upright positions so that you do not tire yourself out. It i s useful to bear in mind that the more vertical or upright your body is the more help you will get from gravity. When standing or walking you may find it helpful to lean forward onto a wall or to be held by your midwife or partner during the contractions.
When kneeling make sure your knees are resting on a soft surface and use a firm beanbag or pile of cushions to make yourself comfortable to relaxing between the contractions and to make sure that your trunk stays fairly vertical.
You may want to rest lying on your side, well propped up by cushions between contractions. For squatting, a low stool is very helpful and makes squatting less tiring. You can also hold onto a firm support or squat between your partner’s knees while he sits on a chair.
Sitting on the toilet with your knees spread apart is very comfortable in labour and for many women the privacy of the bathroom is appealing. Here you can fill the basin and splash yourself with water if you want to and enjoy the sound of running water from the tap.
Entering the Pool
Once you enter the pool, water powerfully increases your sense of privacy and adds a new dimension to the range of positions and movements you can use. The buoyancy of the water makes it much easier to move and change position and you will find that you will change positions instinctively and movement will occur spontaneously.
It’s helpful to experiment in the pool or in a swimming pool in the days before your labour begins, and to submerge your head under water at times so that you feel completely familiar and at ease in the water. This is a way to block out sounds which are distracting.
You will find that most of the movements and positions you can use on land can be used in water during contractions.
Floating between contractions is a wonderful way to relax, and wetting your hair and going under the water at times reduces outside stimulation and sounds and helps you to let go. there is a wonderful sensuous quality to being in water in labour.
It is like reconnecting with the original primal feelings you had in the womb. This is a tremendous aid to surrendering to the birth energy and to letting your body’s natural rhythms take over.
There is no need to do anything. It will help if the room is darkened and you have enough privacy. With the water as deep as possible you can use your ability to relax and quieten your mind to sink deeply into your labour.
Some women remain quite still in the water, changing positions occasionally, whereas others like to move a lot, rolling from front to back like a mermaid, or a dolphin.
Movements and position changes will happen without you needing to think about them. Between contractions you can rest and benefit from the restorative and energising properties of the water.
You can sink into its nurturing and feminine energy and accept its power to relax you. If you can let go completely you will rest, your energy will recharge and you will enter into a kind of timeless ocean of bliss between the contractions.
The End of Labour
As the birth of the baby approaches contractions will be at their most intense. They will be longer (lasting up to sixty seconds) and closer together so that the intervals are very brief.
This is the peak of labour when the ocean waves are high and turbulent, following upon each other with relentless frequency. The end of labour is usually referred to as ‘the transition stage’. You are close to full dilation and your baby’s head is about to emerge through the dilated cervix into your vagina ready to be born.
It is normal to feel fearful at this stage. This is the time when you are likely to wish you could get away or have an epidural anaesthetic, when your courage and strength may be at a very low ebb.
You may feel angry and irritable or despairing, as if you are exhausted and almost close to death. The breaks between your contractions may give you little respite before the next contraction looms large, like a tidal wave.
It is very helpful to make the most of the respite between contractions and rest and relax deeply, almost sleeping until the next wave begins. this can restore and replenish your energy surprisingly – even though the gaps are short.
The fear which is common at this stage has an important role to play. It triggers off a surge of adrenalin secretion, the ‘fight or flight’ hormone which stimulates the reflexive contractions which expel your baby during birth.
At this time you are on the threshold of giving birth. This is when the powerful demon goddess takes over as the urge to bear down and give birth arises.Outside stimulation including sound and light or touch should be minimal, as you go through these last demanding contractions without distraction.
You will be in an altered state of consciousness, deep inside your labour. Anyone who is present will need to be very discreet and avoid disturbing you, by watching, talking or by being falsely reassuring or anxious.
This time can also be difficult for birth attendants and partners who may feel an intense desire to do something to help. However, their calm silence can be a source of strength, reassurance and encouragement as you go through the intensity of the end of labour.
Some women are deeply afraid of the birth at a subconscious level and may experience difficulty in surrendering to the power of these final contractions. Being in warm water helps to let go. Often this intense phase passes very quickly or has a kind of timeless quality.
However, if transition is long, you can keep up your energy by sipping water or dilute fruit juice. Most women feel very thirsty when the adrenalin response begins and need to drink a glass or two of water. The bach flower remedy called ‘Rescue Remedy’ can be very helpful.
At this time near to the birth, the sounds emerging from the birth room tend to be loudest, so there is no need to try to be quiet. You will be in your full power, so feel free to roar like a lioness if you need to .
Noise will help you to find the power to assist your baby to come down as your body opens to give birth. Your bowels empty spontaneously as your baby’s head presses down and you may need to retch as the expulsive reflex begins.
Some women feel shy or inhibited about letting go to to these natural reflexes in the presence of other people. It helps to remember that your midwife is used to this and will welcome these events as a sign that the birth is imminent. Whatever happens your concentration will be focused deeply on the power of your contractions with moments of brief but blissful serenity in between them.
At this stage you may feel that you are almost drowning in a sea of contractions. You may wish to leave the water, or alternatively surrender to the power in the weightlessness which its buoyancy allows you.
Whether you are in or out of the pool, it is best to use the positions which feel most comfortable, making sure that you can relax, with your body supported between contractions. The water level in the pool should be as high as possible to offer you maximal support.
As birth approaches, many women prefer kneeling. This position helps to give you a sense of control over the intensity of the contractions and makes it easier to relax or even sleep in the brief intervals between them without moving or changing position.
At the very end of labour, contractions often slow down and the resting phases may lengthen. The contractions which expel our baby from the womb usually begin around the time full dilation of the cervix is reached.
In some women the urge to push may start before dilation is complete and sometimes, on the other hand, there is a break or resting period before expulsion begins. This will feel like a lull, a period of time where suddenly the waves become still and the sea becomes calm.
The lull may continue for quite a while before the pushing urge begins. On the other hand you may begin to feel the urge to bear down much earlier. Whatever happens you can trust in the wisdom of your body and surrender to its urges. Soon your baby will be born!
When you feel you are ready to push and give birth to your baby you may decide to leave the pool, to feel the solidness and security of the ground underneath you. Or you may prefer to remain in the water for the second stage. Some women have a strong urge to get out, while this possibility may not even occur to others.
In some places, especially when the midwives are new to water birth, pools are used only for labour and all women are asked to get out for the birth.
The benefits of using a pool during labour are the main reason to consider using the help of water. If you are asked to leave the pool to give birth, it is still well worth getting in for labour. The birth often happens very soon after the mother leaves the pool at the end of active labour in water.
A water birth is appropriate when labour has progressed well and when there is no sign of a potential problem during labour. When this is the case, studies have shown that giving birth in water is as safe as any other way of giving birth. A water birth is a soft and gentle way for a baby to be born and welcomed to the world.
Birth in water is a ‘low risk’ option. It is only recommended when the baby’s heart tones are strong throughout labour and second stage and when there are no complications. That’s why your midwife will want to listen in to your baby every half hour or so during labour, and this is done even more frequently in the second stage.
In places where a birth pool is encouraged as an option, women rate the experience of labour and/or birth in water very highly (one study showed that just over 90% of women who had a water birth rated it as ‘excellent’) and research has shown that fewer women need interventions.
Using a birth pool, whether just for labour or for the birth itself, is an effective and harmless way to reduce the risk of complications and to increase your chances of a natural birth.
* The dive reflex – a major discovery
The evidence of many thousands of water births all over the world has shown us that when the circumstances are appropriate, babies can be born safely into warm water at around body temperature and brought immediately to the surface to breathe. This is due to an innate reflex in human newborns called the ‘dive reflex’.
This was first discovered by the Russian researcher Igor Tjarkovsky in the 1960’s and was first described in the medical literature by the eminent neonatal physiologist Paul Johnson, from the John Radcliffe Hospital in Oxford. He is an expert on the first breathing responses of the newborn. In March 1996 he published an article ‘Birth under water- to breathe or not to breathe?’ in the British Journal of Obstetrics and Gynaecology. The dive reflex was also researched by the German obstetricians Eldering and Selke and their findings are published in the book Water Birth Unplugged.
Johnson point out that the breathing reflex in a newborn baby is stimulated at birth, at the moment when the sensory chemoreceptors around the babies nose and mouth first come into contact with air.
When the head emerges into warm water at body temperature during a water birth, this stimulation does not occur before the face emerges from the water. Under water, the dive reflex causes the air passages in the larynx to close and any water entering the nose or mouth is swallowed rather than inhaled.
The only time the dive reflex may be overridden, causing the baby to gasp under water, would be if there was severe foetal distress. This is why diligent monitoring to rule out this possibility is an essential feature of a water labour or birth. Labour and birth in water tends to minimise stress and relax the birthing mother. This in itself is a preventative of foetal distress.
However the death of a baby can occur on rare occasions with any method of birth. Infant mortality during water births that are skilfully managed, appears so far, to be exceptionally low, comparative with the national rate for low risk mothers (which is very low in the UK).
Birth in water
The possibility of your baby being born in water may be very appealing and a water birth is certainly a beautiful, gentle way to welcome your baby. However it may not be appropriate at the time, so try to avoid having too much of preconceived idea about this. Even if you would love to have a water birth, try to keep an open mind.
Water births happen when second stage progresses well and the mother does not want to leave the pool.
The baby usually emerges without difficulty, sometimes the head and body are born in one contraction. Often though, the head is born first and there is a break between contractions when just the baby’s head is out. The dive reflex is working while the head is under water, so the baby will not inhale the water. He or she is still receiving oxygen from the placenta through the umbilical cord. The placenta remains attached and working until the baby is breathing independently.
Usually with the second contraction, after the head has emerged, the shoulders and the body emerge next baby is born into the water. The buoyancy supports the baby’s body in the water and you may see the babies eyes open under water. The dive reflex is still working. The baby is then gently ‘caught’ and brought to the surface immediately.
This is done in slow motion, without rushing, within about 10 seconds after the baby has been born, which gives the baby enough time to relax and uncurl in the water on the way out. The baby is lifted out in time to take the first breath, when the mouth and nose come in contact with the atmosphere.
With this gentle way of birth, breathing usually starts slowly with the baby taking frequent little breaths instead of one big gasp. Within minutes breathing is established and it takes about 10 -15 minutes before the cord stops pulsating altogether and the transition to lung breathing is completed.
Holding your baby in your arms for the first time, is one of the most wonderful experiences you will ever know. No doubt you will kiss and caress your baby and hold him or her close to your heart. Take your time to welcome and enjoy your baby in privacy – this first bonding is the beginning of a love affair which will last a lifetime!
After the birth
While welcoming your baby you can stay in the pool and hold your baby in your arms, close to the breast. Your partner or birth attendants may need to alter the depth of the water to ensure that your baby’s body is submerged and kept warm, while the head is able to reach the breast easily above the water surface.
This is a good moment to put on a heater so the room is very warm when you leave the pool. Facilitating the first undisturbed contact between mother and baby is what is most important now – ‘daddy bonding’ time happens a little later after the placenta has emerged safely. The birth is not over until then.
While doing these practical tasks, try to keep the room very calm and quiet, maintaining privacy so that the mother is not distracted from her baby.
It’s a good idea to encourage the baby to latch on to the breast and to get the first sucking going if possible. This will stimulate more contractions. The cord is usually clamped and cut after it stops pulsating or after the placenta has emerged.
You may be asked to leave the pool when you start to get third stage contractions, so that the placenta is delivered when you are outside the pool. It’s possible to stay in the water while the placenta emerges and many experienced water birth midwives will have no objection. There is no evidence of this being a problem. However, as there is still uncertainty about this, many midwives have to adhere to a policy of the placenta being born on dry land.
The important issue now is not where the placenta emerges, but that first contact with your baby is undisturbed. So if you need to leave the pool, stand up holding your baby. Step carefully out of the pool and sit on a soft surface on the floor (an inflatable swimming ring covered by a soft towel is ideal!). Have someone drape some warm towels or a bathrobe over your shoulders and carry on welcoming and feeding your baby.
The room needs to be warm to the point of ‘over heated’ so the baby is kept very warm by your body heat and the room temperature! A soft warm towel or flannel sheet can be placed over the baby in your arms. Skin-to-skin contact with your baby should be maintained continuously, until the placenta has emerged, as this will enhance bonding and stimulate third stage contractions simultaneously.
These can feel very crampy and it is a great relief to give birth to the placenta, which is softer and smaller than a baby! It’s a surprisingly pleasurable feeling birthing the placenta.
Most women feel ecstatic after a physiological water birth. Babies tend to be calmer and often seem to smile fleetingly, although their face muscles only become strong enough to sustain a smile at around 6 weeks old. They generally settle into life easily with a sense of wholeness and continuity from the shelter of the womb to the close contact with mum after the birth. Many mother’s feel that this is the kindest, gentlest and most loving way to have a baby and that nothing could be more natural. For you and your partner it can be wonderful way to celebrate the birth of your child.
“I got into the pool at 5 cms dilated after approximately 4/5 hours of comfortable early labour at home, having used lots of movement and upright positions. Getting into the pool made me feel very comfortable and much more mobile and seemed to speed up labour. The contractions were very effective and I was fully dilated and ready to push after about 2 hours in the water. Our lovely daughter Lily Martha was delivered into the water after about 40 minutes of pushing and seemed very happy about the whole experience. I got out of the pool for a natural delivery of the placenta. I felt the whole experience of being at home and using the pool was amazing and contributed to a stress-free and wonderful natural birth.”
Melissa Clarke, London N1. First baby born 5th May 2001